3D echocardiography to plan aortic valve surgery and evaluate the results
Abstract
Three-dimensional transesophageal echocardiography (3D TEE) has become an indispensable tool for the anatomical and functional assessment of the aortic valve (AV). Accurately identifying the degree of regurgitation or stenosis is critical for therapeutic decision making; 3D TEE provides comprehensive morphological and functional descriptions, which have been improved by the introduction of new analytic methods. This review examines the development of 3D echocardiography in evaluating AV disorders, emphasizing its advantages over conventional 2D imaging. 3D TEE improves the accuracy of measures crucial to surgical planning and prosthesis selection, enabling real-time visualization of valve shape and dynamics. The widespread adoption of 3D echocardiography will contribute to improving the treatment of AV diseases as technology advances, thereby opening new horizons for more patient-tailored therapeutic strategies.
Keywords
INTRODUCTION
In the past 20 years, reparative cardiac surgery and transcatheter procedures have become increasingly prominent in the treatment of structural heart disease, particularly valvulopathies. Therefore, a comprehensive understanding of the etiology and pathological components is essential for selecting the optimal therapeutic strategy for each patient. Echocardiography, both transthoracic (TTE) and transesophageal (TEE), plays a key role in assessing the anatomy and function of the heart valves. In particular, three-dimensional echocardiography (3DE) represents one of the most significant advances in cardiovascular imaging and has overcome many of the limitations of the two-dimensional (2D) echocardiogram. Indeed, 3D TEE has become critical for procedural planning, intraprocedural guidance, and the assessment of procedural results[1]. This revolution has been made possible by advances in new image rendering methods, software and crystal technology, which have led to innovative array transducers capable of acquiring a pyramidal volumetric dataset rather than a single cross-section displaying 3D echocardiographic images in real time[2]. An inverse relationship exists between volume rate, volume size, and spatial resolution; increasing any one of these parameters decreases the other two. The resolution and accuracy of 3D images are contingent upon multiple factors, including patient-specific acoustic windows and tissue characteristics, the imager’s experience, and, most importantly, the quality of the 2D image. Indeed, the 2D image must be optimized before 3D acquisition.
To obtain an optimal image, the pyramidal volume containing the anatomical structures of interest should be as small as possible. The depth and the elevational and azimuthal planes should be adjusted in biplane mode before the 3D volume is acquired. Acquiring the full 3D volume in a multibeat mode is recommended to increase spatial and temporal resolution[3].
Modalities to acquire a 3D dataset for aortic valve assessment
X-plane imaging is one of the most widely used modalities. Two simultaneous cross-sectional views are obtained from the same heartbeat, with the default images being orthogonal (90°) to each other. Typically, the left sector displays the reference imaging plane, while in the right sector, the rotation angle and position of the secondary plane can be changed. X-plane imaging enables the simultaneous visualization of anatomical structures, thereby improving measurement accuracy[4] [Figure 1]. With the increasing use of aortic valve repair and transcatheter replacement, X-plane imaging has become indispensable for studying the aortic valve (AV) and selecting the optimal treatment. Each leaflet is analyzed in detail in its three distinct anatomical regions (hinge line, body, and lunula) and their interrelationships. Morphological changes in the cusps, such as calcification, prolapse, billowing, and fenestrations, can be described. Cusp parameters (e.g., area, height, length, and depth) should be measured not only for treatment selection but also for estimating the postoperative status[5,6]. Color flow Doppler can be superimposed to define the regurgitant jet origin, direction, and vena contracta (VC)[7].
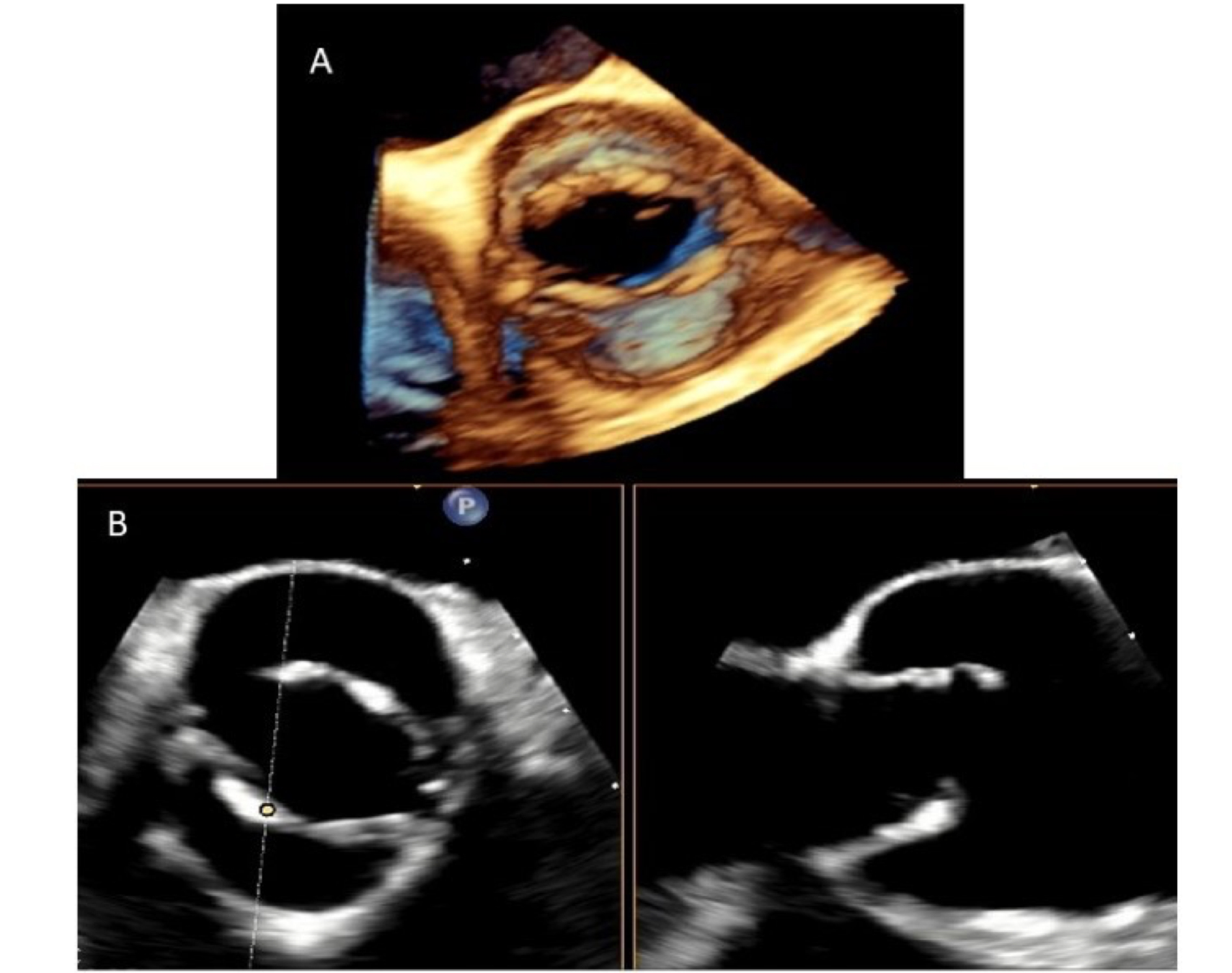
Figure 1. 3D TEE of a BAV in the short-axis (Panel A). X-plane mode at the level of the aortic valve shows BAV without raphe, anteropeposterior phenotype (Panel B). TEE: Transesophageal echocardiography; BAV: bicuspid aortic valve.
The real-time single-beat modality is obtained from the 2D TEE by pressing a single button. It is the most frequently used modality during percutaneous procedures, as it is unaffected by stitching artifacts. The image obtained is a solid pyramidal dataset with a narrow angle (usually 30° × 60°) that can be increased by modifying the azimuthal and elevational planes (up to 90° × 90°). In contrast, the electrocardiogram (ECG)-gated multi-beat acquisition modality is prone to stitching artifacts but has higher spatial and temporal resolution. This acquisition method constructs an image by stitching up to six narrow sectors (subvolumes) and requires a regular heart rhythm and a breath-hold. It is the optimal method for detailed anatomical and functional analysis of the aortic root and AV. Color Doppler can be added in both modalities, but it reduces the frame rate[2] [Table 1].
Comparison of 3D echocardiographic acquisition modalities
| Acquisition modality | Advantages |
| X-plane | Displays two views from the same heartbeat using a single acoustic window. The default views are orthogonal (90°) to each other |
| Real-time single-beat | Free from stitching artifacts; commonly used during percutaneous procedures |
| ECG-gated multi-beat | May exhibit stitching artifacts but offers higher spatial and temporal resolution |
| 3D color Doppler | Enables 3D flow imaging but reduces the frame rate |
Regardless of the acquisition mode, it is important to consider how 3D structures are displayed on a 2D screen. There are different 3D image displays:
Volume rendering uses various algorithms to preserve all 3D information. Various shades of a blue-bronze combination are used to generate a 3D display of the depth and textures of cardiac structures. The 3D dataset can be sectioned, cropped, and rotated[8] [Figure 2].
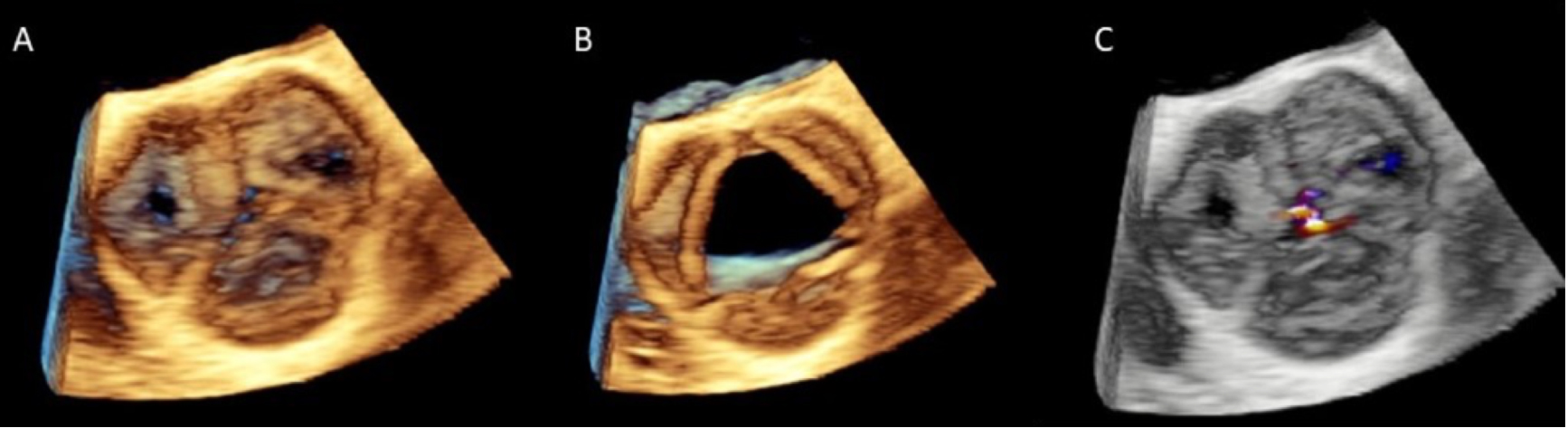
Figure 2. Multi-beat 3D TEE acquisition in zoom modality of the AV in diastole (Panel A) and systole (Panel B). 3D TEE mid-esophageal short-axis view with color-flow Doppler demonstrates moderate AR with a central origin (Panel C). TEE: Transesophageal echocardiography; AR: aortic regurgitation.
Surface rendering enables the visualization of organ surfaces with a solid appearance, through manual or semi-automatic boundary tracing. These automated algorithms utilize forms of artificial intelligence to identify fiducial anatomical landmarks.
2D Tomographic Slices show multiple simultaneous 2D views of the single pyramidal dataset. Multiple slicing methods are available, such as arbitrary plane, simultaneous orthogonal (or arbitrary angle) slices, and parallel slice planes.
Photorealistic vision (true-view) with Glass is the newest volume rendering mode, with editing tools such as transparency and light source manipulation. Transparency allows the user to navigate through cardiac structures while retaining anatomical landmarks and overlying tissues. Light source manipulation permits backlighting the anatomical structure of interest to enhance contrast and refine borders. This photorealistic imaging offers more natural and realistic images, facilitating the detection of fine-drawn structures and pathologies[9].
Multiplanar reconstruction (MPR) of acquired 3D datasets is the most accurate rendering mode for performing measurements. Initially, this technique was used after the acquisition of 3D datasets; currently, live MPR is available, which improves the accuracy of real-time measurements through the simultaneous visualization of cardiac structures in multiple planes[10] [Figure 3]. Specifically, live 3D MPR simultaneously displays the structure of interest in the three spatial planes (axial, coronal, and sagittal), enabling a more detailed assessment of cardiac structures than biplane imaging alone. With MPR, the imager can manipulate three distinct 2D sections of a 3D volume as needed. MPR is widely established for planning and guiding transcatheter procedures. For the AV, however, it is the cornerstone for patient selection and for predicting the likelihood of a successful repair. Understanding the interaction between the leaflets, annulus, commissural structures, and sinotubular junction (STJ) allows the surgeon to propose a tailored repair for isolated aortic regurgitation (AR). MPR is the optimal method for quantifying AR by reconstructing the 3D VC area, assessing leaflet tissue quality (i.e., grading thickening and calcification), and defining specific measurements of leaflet geometry, such as coaptation height (cH), effective height (eH), geometric height (gH), and free margin length[11].
Figure 3. Glass (transparency) allows the imager to adjust the degree of transparency of both cardiac and extra-cardiac structures (Panel A). Multiplanar reconstruction allows live rotation of perpendicular planes on a 3D image to display any desired 2D imaging plane (Panel B). 2D: Two-dimensional; 3D: three-dimensional.
However, 3DE has some limitations. Its accuracy depends on image quality: a poor acoustic window can result in suboptimal 3D acquisitions and artifacts (e.g., stitching errors). Furthermore, 3DE is an
4D TEE produces realistic, easily interpretable images. It enables the acquisition of a large amount of information in a single step, constructing multidimensional images from the same heartbeat without requiring probe movement. It provides real-time color flow to assess hemodynamic information within the same cardiac cycle, which is particularly useful for quantifying valvular regurgitation. We use 4D TEE in candidates for transcatheter aortic valve replacement (TAVR) or valve-in-valve procedures who have kidney disease and may not have undergone adequate multidetector computed tomography (MDCT), or in patients with poor-quality MDCT for whom annular dimensions require confirmation[12].
THE ROLE OF 3D ECHOCARDIOGRAPHY FOR AORTIC VALVE STENOSIS ASSESSMENT
Aortic stenosis (AS) is the most prevalent valvular heart disease, largely as a consequence of an aging population[13]. Echocardiography is the gold standard for confirming the diagnosis, estimating severity, and establishing indications for intervention. Current international recommendations for the echocardiographic evaluation of patients with AS are mainly based on peak transvalvular velocity, mean pressure gradient, and valve area assessment evaluated by TTE[14], using the simplified Bernoulli equation: ΔP max = 4V max2[15].
From an interventional perspective, accurate preoperative measurement of the aortic annular diameter is crucial for selecting a suitable prosthesis, and TEE is one of the most useful tools. Several studies have shown that measurements by 3D TEE and MDCT have better accuracy than 2D TEE in assessing the aortic annulus[16-18].
Compared with MDCT and cardiac magnetic resonance (CMR), 3D TEE has several advantages: (1) it can be performed in real time, enabling intraprocedural evaluation during surgical aortic valve replacement (SAVR) or as an intraprocedural guide during TAVR; (2) it clarifies the etiology of AS (e.g., calcific, degenerative, or rheumatic); (3) it does not require iodinated contrast, making it useful for patients with chronic kidney disease and elderly patients; and (4) it enables the prompt evaluation of procedural complications, such as annular rupture, transvalvular or paravalvular regurgitation, and pericardial effusion.
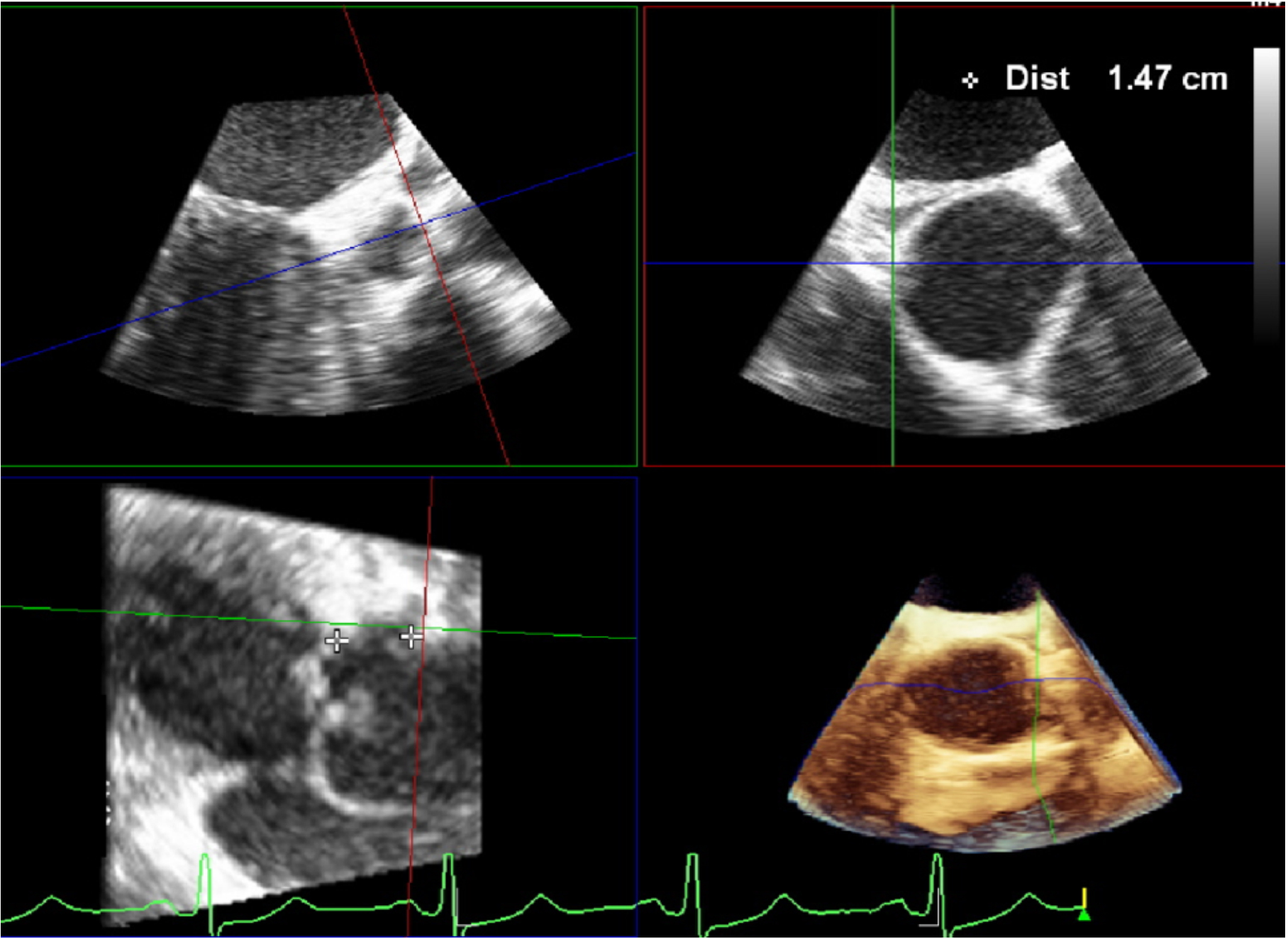
A comprehensive evaluation of severe AS includes the assessment of the diameters and area of the virtual basal ring (VBR). The aortic annulus is a complex, crown-shaped structure. The VBR, a plane connecting the nadirs of the cusp insertion lines, represents its caudal border, while the STJ marks its cranial extent. Thus, the VBR is virtual, and it varies in shape and size, typically being elliptical in diastole and becoming more circular and larger in systole. Interestingly, studies showed that in severe AS, the aortic annulus becomes less distensible and undergoes remodeling, leading to an ovoid shape[19]. Due to calcium shadowing, 2D echocardiography may underestimate the left ventricular outflow tract (LVOT) size, potentially leading to inaccurate measurements of the AV functional area. 3D TEE may overcome this limitation by allowing for direct planimetry of the LVOT area, which is more accurate than relying on a single diameter measurement. Furthermore, 3DE properly delineates non-circular anatomy, which has implications for the correct assessment of AS severity when calculated by the continuity equation, a method that assumes a circular annulus [Figure 4].
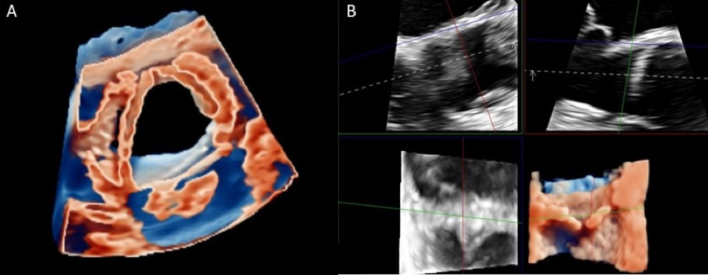
Figure 4. Annular evaluation begins by acquiring a high-quality 2D mid-esophageal short axis (30°-60°) or long axis (110°-120°) image, then selecting the 3D single-beat “zoom modality”. Choose the mid-systolic frame for measurements, as the aortic root is more circular during systole. The sagittal and coronal planes must bisect the AV long axis. The cross-sectional plane should be positioned at the ventricular-aortic junction, with the transverse plane adjusted to display the VBR. 2D: Two-dimensional; 3D: three-dimensional; AV: aortic valve; VBR: virtual basal ring.
Peak transvalvular velocity and mean pressure gradient are flow-dependent parameters, so they can be significantly influenced by cardiac output states, which may potentially lead to inaccurate assessments of valve stenosis severity. The AV functional area is a relatively flow-independent variable that can be calculated using the Bernoulli continuity equation.
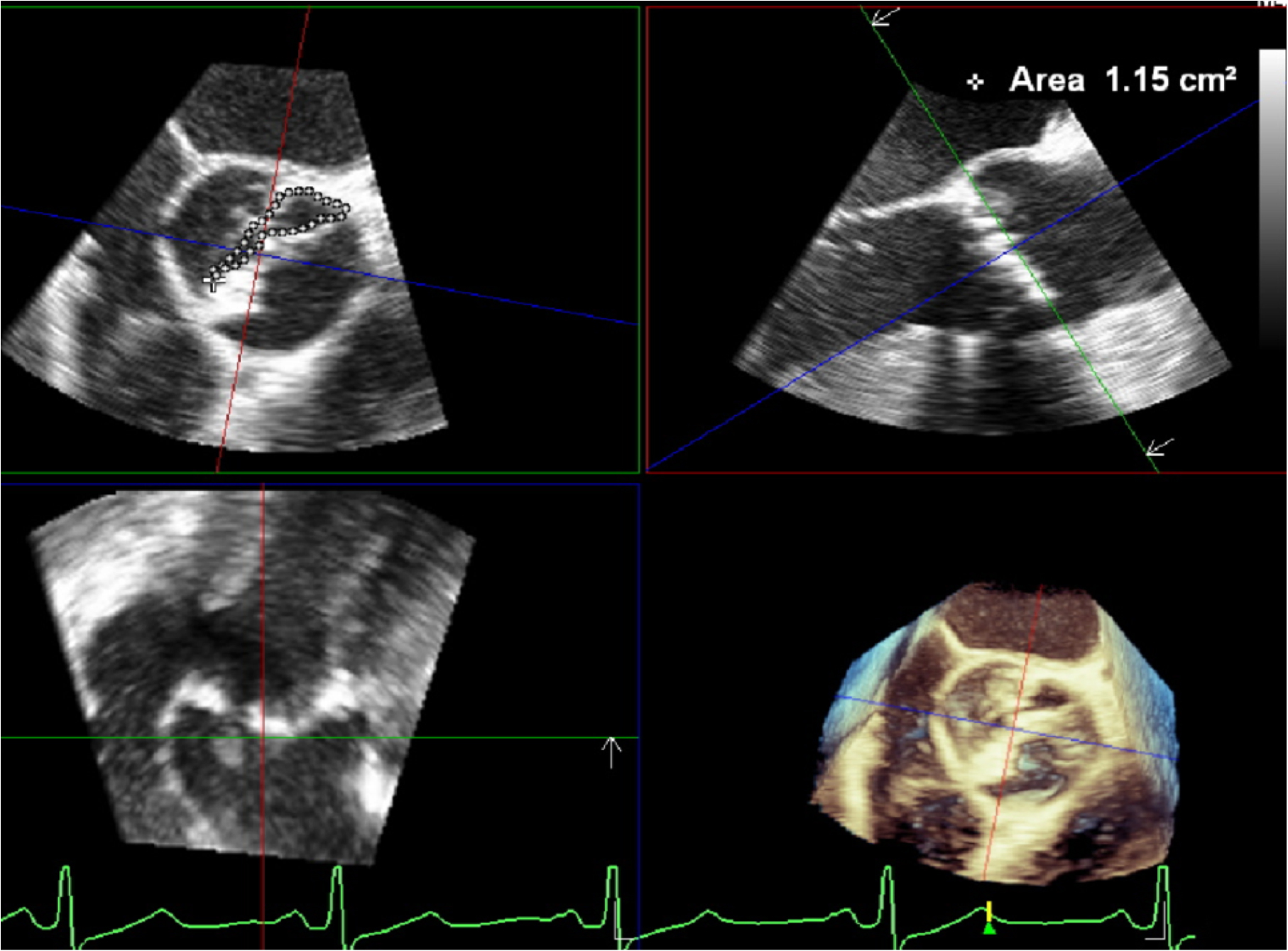
Using a flow-independent method, such as planimetry, to calculate the aortic valve area (AVA) is essential, especially for intraoperative evaluation under general anesthesia[20]. In 2D methods, it may be difficult to detect the tips of the AV leaflets at peak systolic opening for AVA planimetry calculation; this can result in an overestimation of AVA due to a ‘funnel’ configuration. TEE should be considered the echocardiographic modality of choice for calculating AVA planimetry. 3D TEE is more effective than 2D planimetry for assessing AVA[21] and correlates better with continuity equation-derived AVA[22]. Consequently, 3DE improves accuracy and provides a validated alternative to MDCT and CMR for accurate sizing of both the aortic annulus and AVA [Figure 5].
Figure 5. 3D image planes are carefully repositioned towards AV leaflet tips during the mid-systolic phase of the cardiac cycle. This repositioning allows for generating a short axis MPR, where planimetry can be precisely traced to determine the AV area. 3D: Three-dimensional; AV: aortic valve; MPR: multiplanar reconstruction.
FOCUS ON TAVR PROCEDURE: FROM THE PROSTHESIS SELECTION TO THE POST-PROCEDURAL ASSESSMENT
Randomized clinical trials have established SAVR and TAVR as complementary treatment options. TAVR was initially performed as an alternative to SAVR in patients with high surgical risk[23,24]. Recent trials have shown that TAVR is non-inferior to SAVR in low-risk patients at 5-year follow-up[25,26]. However, the lack of long-term outcomes regarding structural valve deterioration creates uncertainty about TAVR durability, particularly in younger patients, for whom re-intervention might be a future concern. Thus, TAVR is a valid alternative to conventional SAVR, especially in elderly patients with favorable anatomical and procedural characteristics[27], while SAVR remains more suitable for patients with a bicuspid aortic valve (BAV) and AS, as well as those with associated disease (e.g., aortic dilatation, complex coronary disease, or severe mitral regurgitation requiring a surgical approach).
While preoperative imaging assessment for TAVR primarily relies on MDCT[28,29], 3D TEE serves as a useful tool to assess valvular size, monitor the procedure, and provide real-time evaluation of procedure results. The first step in planning the TAVR procedure is to correctly measure VBR to avoid complications that can affect short- and long-term outcomes. A recent meta-analysis[30] demonstrated a strong correlation between the LVOT area, aortic annular area, perimeter, and diameter measured using 3D TEE and those obtained from MDCT. Thus, 3D TEE remains a valid alternative for LVOT and VBR quantification, especially when MDCT is contraindicated.
Dynamic changes in the aortic annulus during the cardiac cycle could lead to misinterpretation of annular sizing for prosthesis selection[31]. As the annulus becomes progressively more elliptical, the area decreases disproportionately to the perimeter, leading to potential underestimation of annular size. For accurate prosthesis selection, perimeter-derived measurement of VBR correlates well with the manufacturer’s prosthesis sizing charts and predicts accurate prosthesis size[18]. Annular shape and perimeter are not the exclusive factors for valve choice: each component of the aortic root, including STJ, aortic sinuses, LVOT, and coronary ostia height, is crucial in determining what type and size of prosthesis is appropriate. The intentional oversizing of implants is a recognized strategy to reduce the risk of paravalvular regurgitation (PVR)[32], but it can negatively affect outcomes such as the risk of root rupture, significant conduction disturbances, and device underexpansion.
One of the most feared complications during TAVR is myocardial ischemia due to coronary ostia occlusion. This occurs when a very high prosthesis deployment causes the calcified native leaflets to be crushed against the aortic wall by the expanding metallic stent frame. MDCT is the gold-standard tool for evaluating coronary ostia height[33,34]. Although 3D TEE is not the primary modality for measuring coronary height, a good correlation exists between TEE (including with 4D software reconstruction) and MDCT in estimating left coronary height[35]. The right coronary ostium can be identified through a 2D TEE mid-esophageal
Figure 6. Combine the sagittal and coronal images to cut the AV long axis. In the sagittal plane, search for an indentation at the 10 o’clock position, which represents the left main coronary origin. Then move the marker along the aortic root in coronal view. Rotate the marker in the transverse image anticlockwise until it is perfectly aligned with the left major ostium. Finally, carefully measure the distance between the left main ostium and the left cusp in the sagittal plane. AV: Aortic valve.
Real-time imaging guidance throughout implantation offers prompt diagnosis of complications and indicates the proper landing zone. In the short-axis view, the prosthesis must be circular, and the proximal edge must be a few millimeters inside the LVOT, without significant protrusion. In the case of a suboptimal result, self-expanding prostheses can be repositioned, while balloon-expandable ones may require
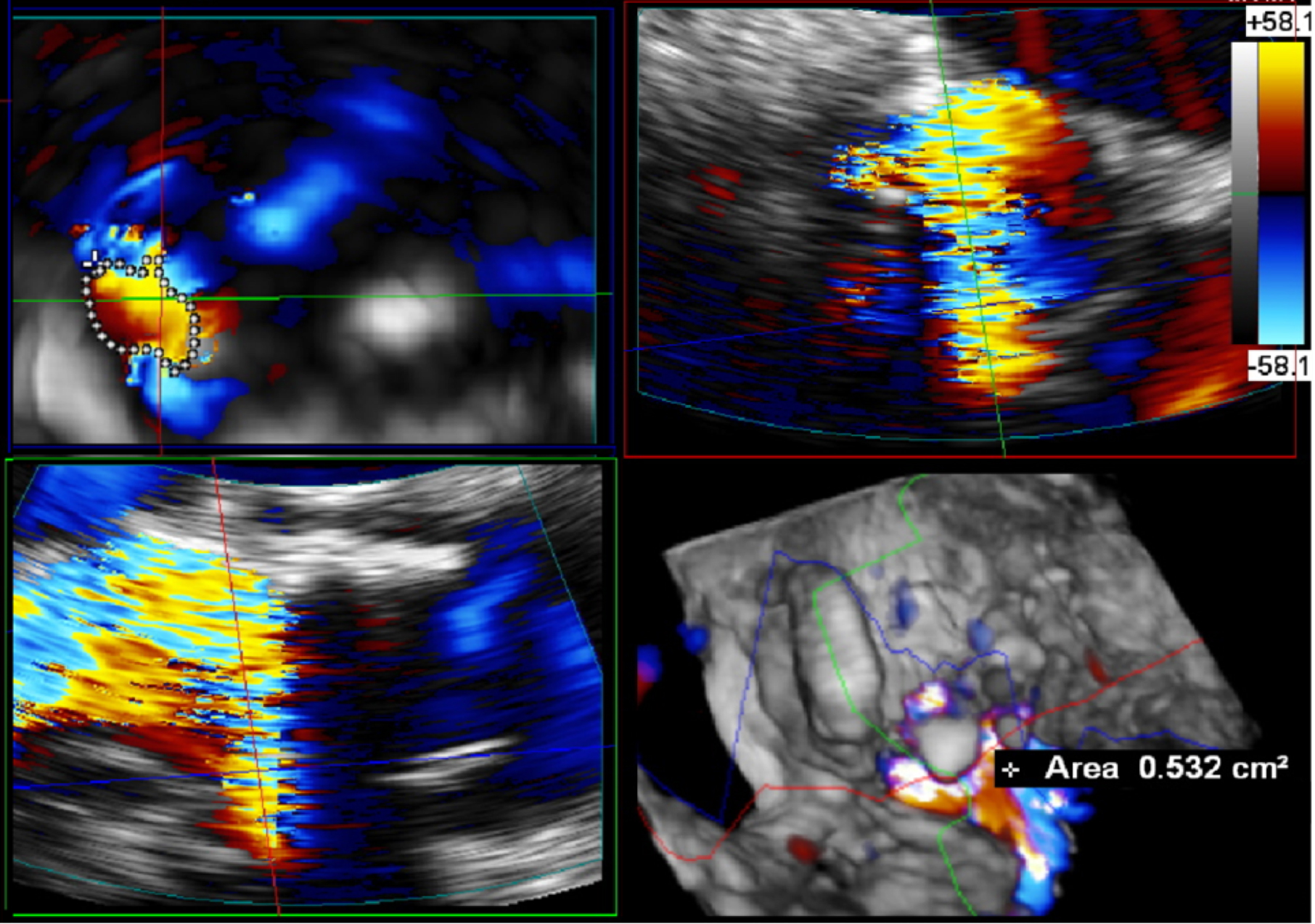
After proper deployment, PVR and intravalvular leaks must be excluded. Transvalvular leaks are primarily associated with incomplete stent frame expansion, an elliptical prosthetic shape, and malpositioning[37]. Prosthetic expansion assessed by 3D TEE was defined as the ratio of the mid-edge area of the prosthetic frame to the nominal external valve area, and this ratio was significantly higher in patients with transvalvular AR. PVR remains the most frequent complication of TAVR. Moderate or severe PVR is an independent predictor of mortality after TAVR implantation. MDCT and 3D TEE predicted PVR with similar accuracy[38] [Figure 7].
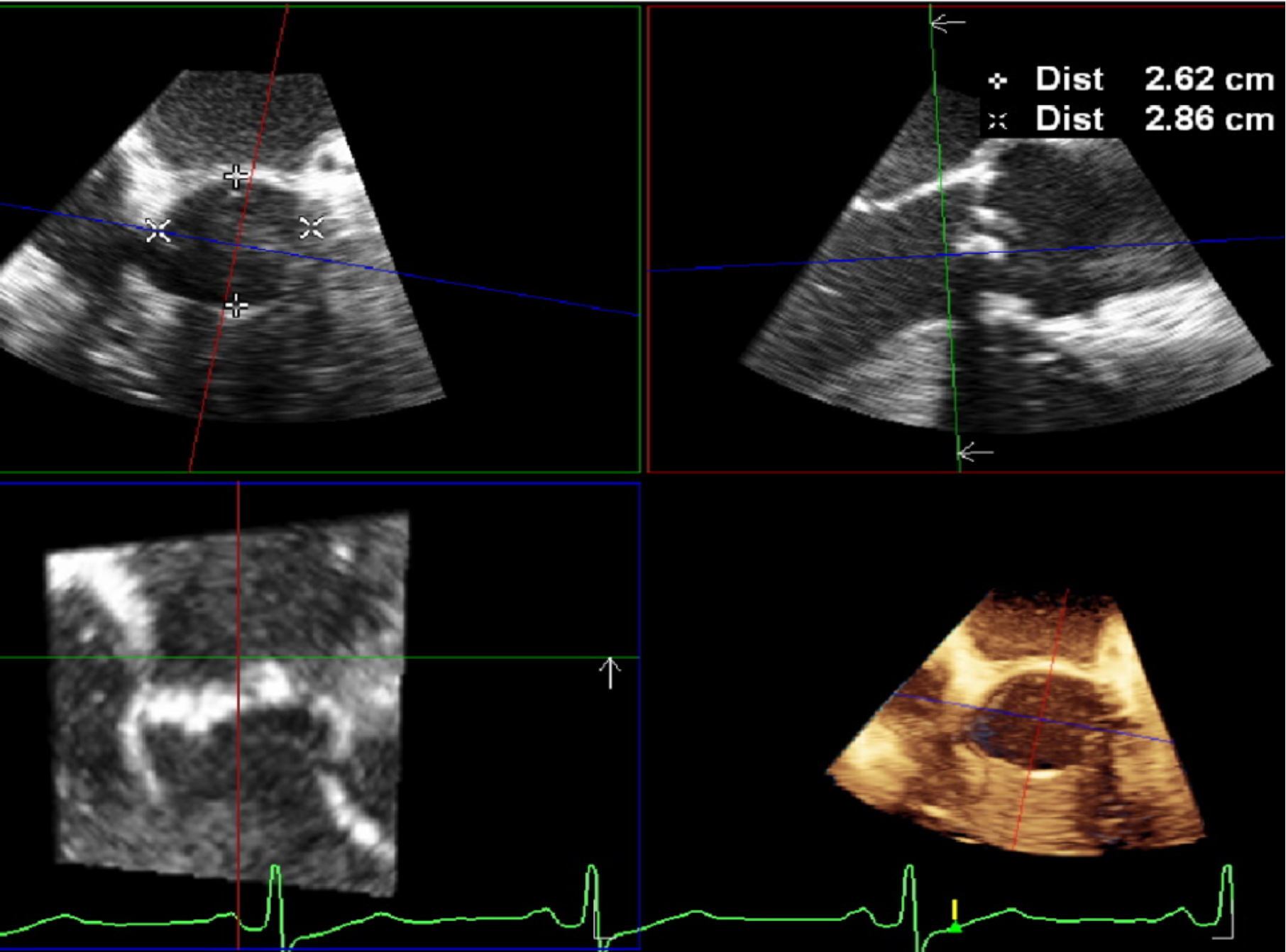
Figure 7. Following AV short-axis imaging, a 3D “zoom modality” with color is applied. The resulting image is presented in four distinct portions: sagittal, coronal, transverse, and whole-volume render. The diastolic frame is carefully selected for optimal visualization. To comprehensively demonstrate the paravalvular leak, the sagittal and coronal planes must be precisely bisected in the transverse plane. By methodically tracing the circular path, a 3D VC of the paravalvular leak can be generated. It is important to note that regurgitation is classified as severe when the VC area exceeds 0.3 cm2. 3D: Three-dimensional; VC: vena contracta.
SAVR: OLD BUT STILL GOLD
Similar to TAVR, accurate preoperative measurement of the aortic annular diameter is crucial for selecting the appropriate prosthesis size to avoid patient-prosthesis mismatch (PPM)[39], which negatively impacts short- and long-term outcomes[40,41]. Predicting PPM before surgery is critically important. In fact, after selecting the prosthesis model and size, the predicted indexed effective orifice area (EOA) must be calculated to estimate the risk of postoperative PPM. A predicted indexed EOA ≤ 0.65 cm2/m2 (or
AORTIC REGURGITATION: MECHANISM AND ASSESSMENT FOR VALVE REPAIR PLANNING
AR is a condition caused by various etiologies, including degenerative AV disease, congenital abnormalities, infective endocarditis, and most commonly, aortic root dilatation. The accurate assessment of AR severity is crucial for appropriate patient management and timing of intervention. In the thorough assessment of AR, 3D echocardiography offers significant methodological advantages over traditional 2D imaging techniques. Currently, the multimodality imaging approach is mandatory to establish diagnosis, identify complications, and determine the appropriate surgical treatment. The most common treatment is still AV replacement. Conversely, valve repair and valve-sparing procedures are increasingly adopted, especially for AVs with structurally normal leaflets. Therefore, 3D echocardiography, alongside MDCT, is becoming increasingly important in assessing the feasibility of AV repair. This surgical option is still underutilized but represents a valid alternative to prosthetic replacement and should be recommended when feasible[47]. A standardized echocardiographic assessment protocol is required to select patients with suitable characteristics for repair[48,49] and make this surgical option reproducible[50] with excellent long-term durability[51].
First, it is essential to understand the mechanism of AR. While 2D TEE views permit useful measurements, 3D images provide a more comprehensive view of the AV anatomy, focusing on a detailed assessment of leaflet morphology, coaptation, and the dynamic nature of the regurgitant orifice. Volumetric datasets acquired by 3D echo enable the reconstruction of the AV in multiple planes, facilitating the identification of specific anatomical abnormalities that contribute to AR[52]. One of the key advantages of 3D echo in surgical planning is its ability to provide a “surgeon’s view” of the AV[53], enabling a complete assessment of valve configuration and detecting anatomical or functional cusp abnormalities-such as prolapse, flail, fenestrations, or retraction-which is critical for identifying the AR mechanism[54].
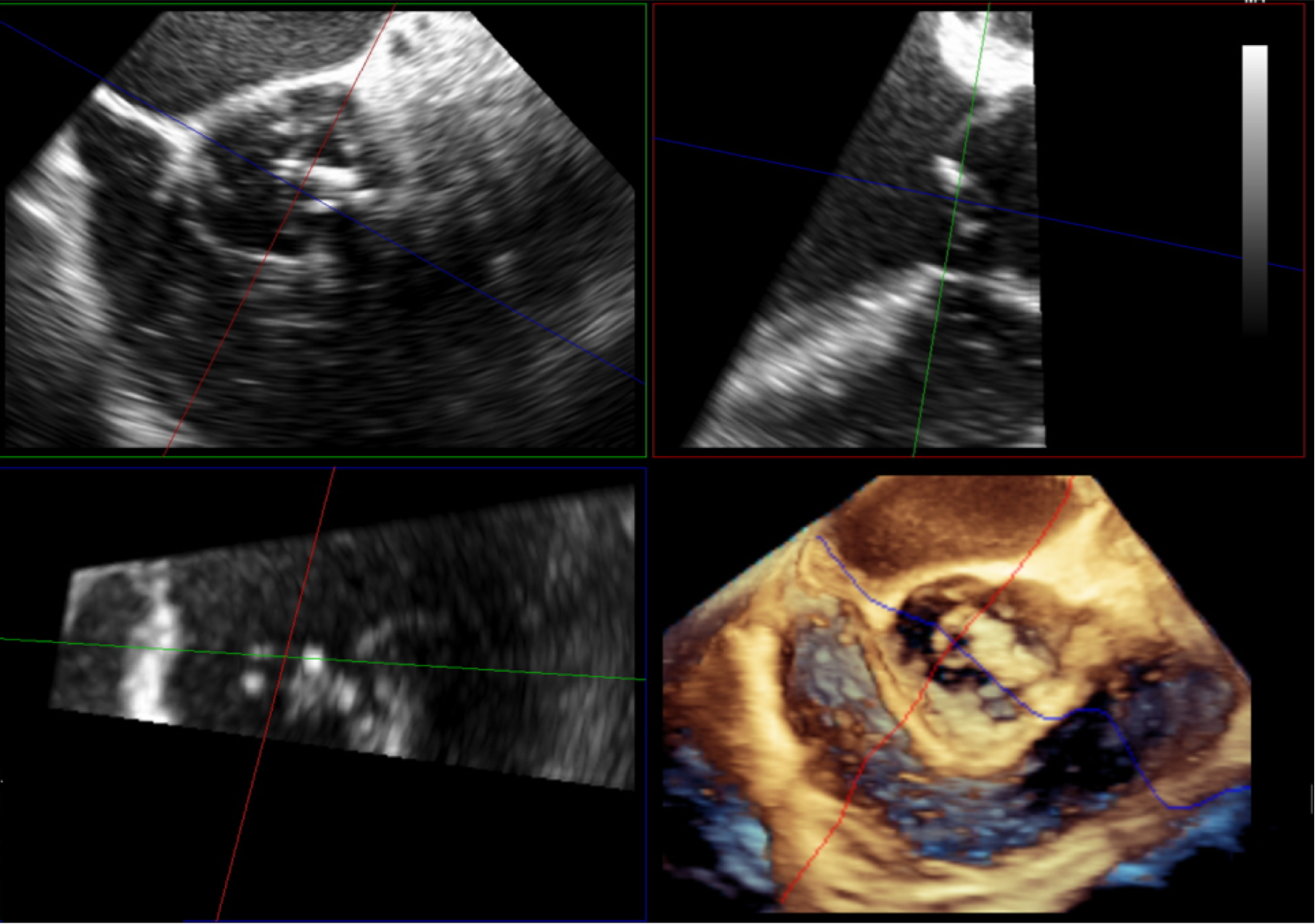
Cusp prolapse is a common cause of AR. Prolapse can be missed by 2D echo, especially if only the left cusp is involved, due to limitations of imaging alignment in long-axis views. Therefore, MPR reconstruction or X-plane imaging should be performed if eccentric AR jets are found[55]. MPR imaging, derived from
Figure 8. MPR reconstruction of BAV with severe AR provides a detailed assessment of conjoint cusp prolapse. MPR: Multiplanar reconstruction; BAV: bicuspid aortic valve; AR: aortic regurgitation.
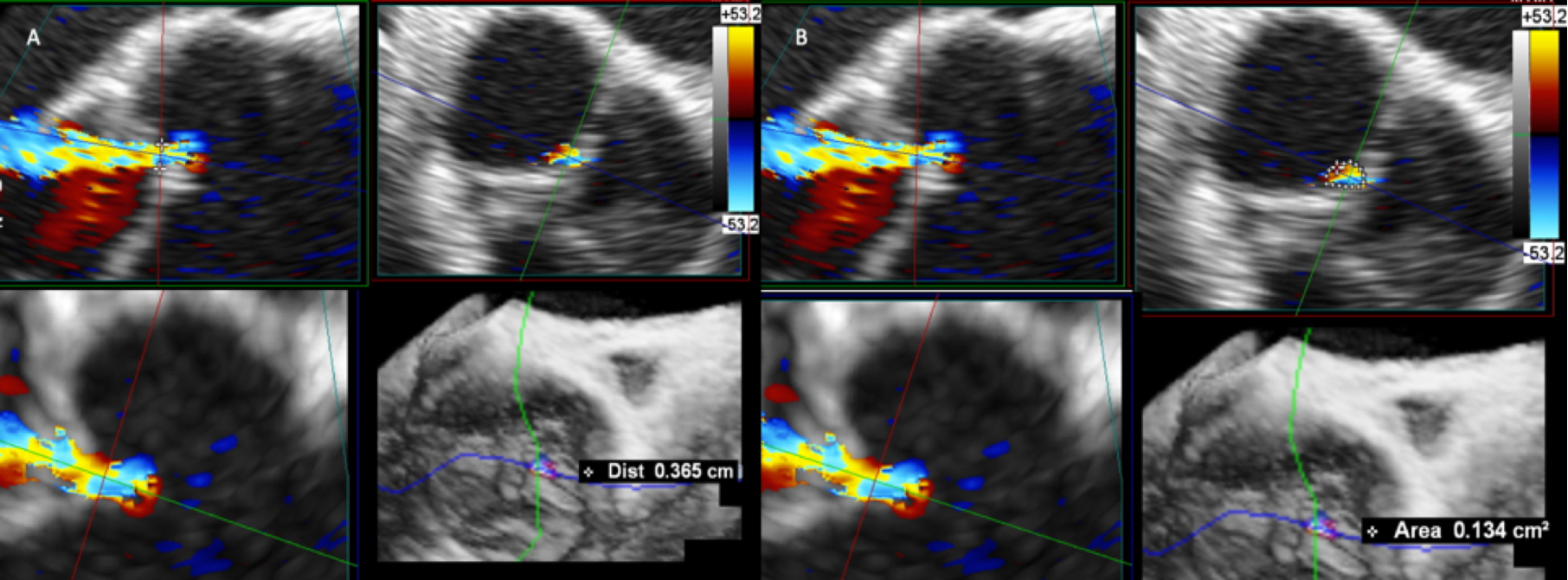
AR severity assessment using 3D echocardiography involves both qualitative and quantitative measures. Qualitatively, 3D color Doppler imaging enhances the understanding of the regurgitant jet’s spatial distribution and its relationship with adjacent structures. This is particularly useful for eccentric jets, the severity of which may be underestimated by 2D approaches[56]. Quantitatively, 3D echo enables direct planimetry of the VC area, a measure that correlates strongly with Effective Regurgitant Orifice Area (EROA)[57]. Unlike 2D, 3D echocardiography can accurately measure non-circular and irregularly shaped regurgitant orifices, providing a more precise assessment of AR severity and showing a superior correlation with invasive measures compared to 2D parameters[58] [Figure 9]. Clinical decision making depends on the precise measurement of regurgitant volume (RVol). 3D echocardiography has significantly enhanced RVol measurement, providing new and more accurate quantification techniques[59]. Ewe et al. conducted an innovative study that compared RVol derived from 3D with that acquired from CMR, which is recognized as the gold standard. The study found that 3D echo measurements outperformed 2D echo methods in terms of correlation with CMR values[60]. Using this methodology, AR severity grading is classified based on EROA and/or RVol, with severe AR defined for an EROA ≥ 30 mm2 or an RV ≥ 60 mL[56].
Figure 9. Determination of 3D VCA using multiplanar reconstruction in the 3D color Doppler dataset. In panel A, the 2D VC measure obtained by MPR orthogonal alignment to AR jet. In panel B, cross-sectional plane through the VC with direct planimetry of VC area. 3D: Three-dimensional; VC: vena contracta; MPR: multiplanar reconstruction; AR: aortic regurgitation; VCA: vena contracta area.
3D echo also enables the calculation of RVol using the difference between the total stroke volume derived from 3D LV volumes and the forward stroke volume measured by Doppler across the LVOT[61]. Moreover, to quantify RVol directly, 3D color flow quantification techniques have also been developed. These techniques determine the flow rate and volume during the cardiac cycle by semi-automatically analyzing the 3D color Doppler information. Shanks et al. showed that this 3D color flow quantification method is more accurate and reproducible compared to 2D approaches, and it has an excellent intraclass correlation coefficient, indicating low interobserver variability[62]. RVol quantification using 3D TEE presents certain challenges: the accuracy of measurements may be affected by variables such as temporal resolution, gain modifications, and Nyquist limit settings. However, many of these issues have been addressed by recent developments in image acquisition and analysis software, enhancing measurement accuracy[63].
Although 3D is widely used in the evaluation of AR, in some cases, such as those with limited acoustic windows, eccentric and/or multiple regurgitant jets, or complex outflow tract geometries, it can be challenging to quantify the severity of the valvulopathy precisely. CMR provides precise,
3D echocardiography enables the precise measurement of three critical parameters that are fundamental for valve-repair assessment and have become a cornerstone of the preoperative, intraoperative, and postoperative evaluation:
Effective height: which is defined as the vertical distance from the annular plane to the free margin of each cusp during diastole. Normal values are about 9 mm to 19 mm[66].
Geometric height: characterized as the curved length of each cusp during diastole from its point of insertion at the nadir of the sinus to the free margin; it defines the amount of cusp tissue substrate for repair. Normal values are above 17 mm to 18 mm in the tricuspid aortic valve (TAV) and 20 mm in the BAV[67].
Coaptation length: which refers to the degree of overlap of cusp tissue in diastole. Normal values are about
Definitions and clinical relevance of key parameters in aortic valve assessment by 3D echocardiography
| Parameter | Description | Clinical relevance |
| Geometric height (gH) | The curvilinear distance from the leaflet attachment(nadir) to the leaflet free edge. It is measured in diastole. It represents the amount of cusp tissue | Crucial for assessing intrinsic leaflet pathology. Reduced geometric height can be seen in restrictive leaflet, often due to calcification or fibrosis, contributing to aortic stenosis or impaired coaptation in regurgitation. A sufficient amount of tissue is essential for valve repair techniques |
| Effective height (eH) | The orthogonal distance from the VBR plane to the coaptation plane of the cusps in diastole. It represents the functional height available for leaflet coaptation | Preoperative negative eH suggests the presence of leaflet prolapse. A key indicator of post repair leaflet competence permits to exclude residual prolapse |
| Coaptation length (cL) | The length of overlap between the opposing leaflets at the coaptation point when the valve is fully closed | Post-repair quantitative parameter that directly reflects the efficacy of leaflet closure. After valve repair a short coaptation length indicates poor leaflet apposition, increasing the likelihood of repair failure |
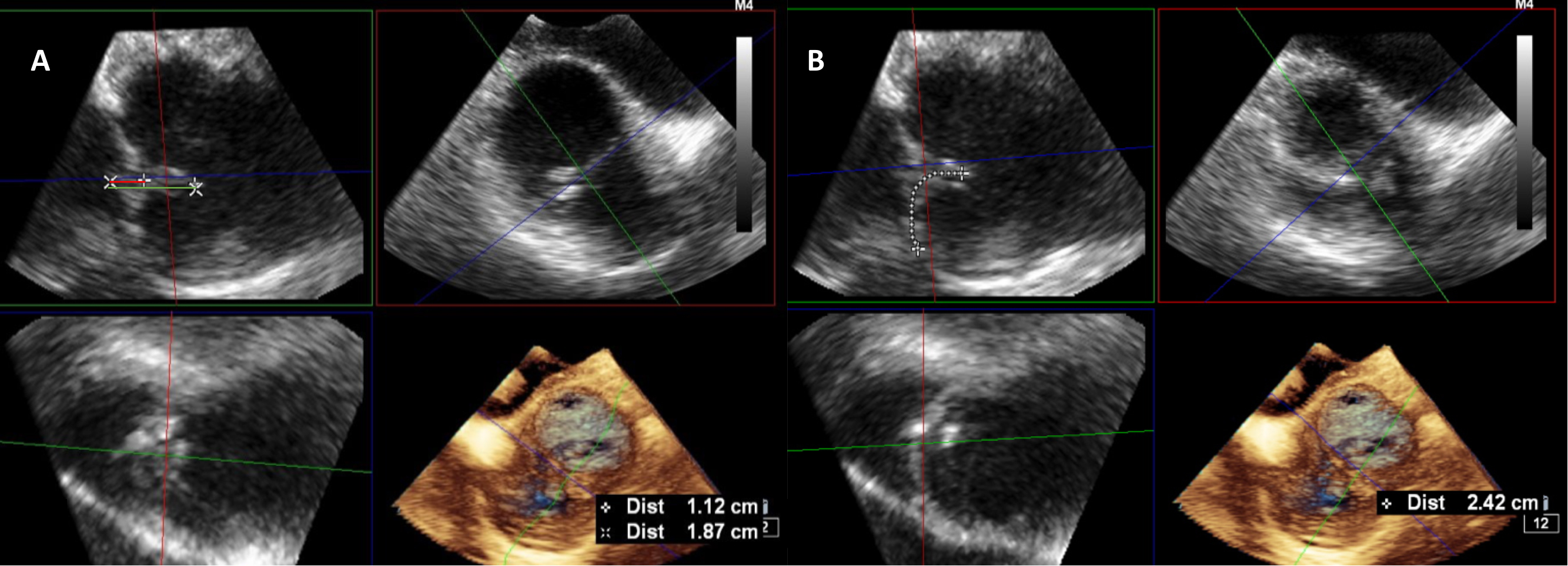
These measurements should be obtained using specific sectional planes during the diastolic phase, created by processing 3D datasets, and should be performed on all three cusps in TAVs. In BAVs, these measurements are typically made only on the non-fused cusp due to the marked heterogeneity of the fused cusp[69]. The gH cannot be correctly measured using 2D echocardiography in TAVs, because the measurement requires an orthogonal plane to the central part of the cusp[70] [Figure 10]. In cases of
Figure 10. The eH, gH, and cL in TAV can be properly determined by measuring the distances between the right and non-coronary cusps, the non-coronary cusp and the left coronary cusp and the left and right coronary cusps. This is accomplished with a plane near the center of the aortic valve. In patients with BAV, both cL and eH must be examined in a plane perpendicular to the commissures and near the center of the valve (panel A), whereas gH should be examined in a sectional plane perpendicular to the center portion of both cusps (panel B). eH: Effective height; gH: geometric height; cL: coaptation length; TAV: tricuspid aortic valve; BAV: bicuspid aortic valve.
Finally, 3D echo facilitates the assessment of LV volumes and function, which are crucial in determining the hemodynamic impact of AR[5]. In clinical practice, 3D echocardiography, particularly with automated software quantification, is essential for detecting LV remodeling and subclinical dysfunction[74]. Subclinical and potentially irreversible cardiac damage can occur in clinically well-compensated patients awaiting surgery. This may be averted by using multimodality imaging parameters, specifically left ventricular global longitudinal strain and CMR[75].
The role of 3D echocardiography extends beyond preoperative planning. Intraoperative 3D TEE is also a valuable tool for real-time decision making during AV repair procedures[76]. 3D color Doppler techniques can precisely locate and quantify any residual regurgitation[77]. Post-repair valve function, assessed by parameters such as cL and eH, is crucial. An eH greater than 9 mm is usually associated with a durable repair and a low risk of significant recurrent regurgitation[78]. An eH below 4 mm is associated with a higher risk of repair failure[7].
CONCLUSION
3D echocardiography has transformed the assessment, management, and follow-up of patients with AV disease. From the initial diagnosis and evaluation of severity to surgical planning and post-repair assessment, 3D echocardiography offers unparalleled insights into both the anatomy and function of the AV. As technology advances, the role of 3D echocardiography is expected to expand even further, potentially enhancing patient outcomes through more personalized and timely interventions.
DECLARATIONS
Authors’ contributions
Conceptualization: Italiano G, Belli M, Lassandro Pepe F
writing-original draft preparation: Italiano G, Belli M, Lassandro Pepe F
writing-review and editing: Italiano G, Belli M, Lassandro Pepe F
All authors have read and agreed to the published version of the manuscript.
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2025.
REFERENCES
1. Surkova E, Muraru D, Aruta P, et al. Current clinical applications of three-dimensional echocardiography: when the technique makes the difference. Curr Cardiol Rep. 2016;18:109.
2. Faletra FF, Agricola E, Flachskampf FA, et al. Three-dimensional transoesophageal echocardiography: how to use and when to use-a clinical consensus statement from the European Association of Cardiovascular Imaging of the European Society of Cardiology. Eur Heart J Cardiovasc Imaging. 2023;24:e119-97.
3. Hagendorff A, Evangelista A, Fehske W, et al. Improvement in the assessment of aortic valve and aortic aneurysm repair by 3-dimensional echocardiography. JACC: Cardiovasc Imaging. 2019;12:2225-44.
4. Fan Y, Chan JSK, Lee AP. Advances in procedural echocardiographic imaging in transcatheter edge-to-edge repair for mitral regurgitation. Front Cardiovasc Med. 2022;9:864341.
5. Piazza N, de Jaegere P, Schultz C, Becker AE, Serruys PW, Anderson RH. Anatomy of the aortic valvar complex and its implications for transcatheter implantation of the aortic valve. Circ Cardiovasc Interv. 2008;1:74-81.
6. Underwood MJ, El Khoury G, Deronck D, Glineur D, Dion R. The aortic root: structure, function, and surgical reconstruction. Heart. 2000;83:376-80.
7. le Polain de Waroux JB, Pouleur AC, Robert A, et al. Mechanisms of recurrent aortic regurgitation after aortic valve repair: predictive value of intraoperative transesophageal echocardiography. JACC Cardiovasc Imaging. 2009;2:931-9.
8. Lang RM, Badano LP, Tsang W, et al. American Society of Echocardiography; European Association of Echocardiography. EAE/ASE recommendations for image acquisition and display using three-dimensional echocardiography. Eur Heart J Cardiovasc Imaging. 2012;13:1-46.
9. Fiore G, Gaspardone C, Ingallina G, et al. Accuracy and reliability of left atrial appendage morphology assessment by three-dimensional transesophageal echocardiographic glass rendering modality: a comparative study with computed tomography. J Am Soc Echocardiogr. 2023;36:1083-91.
10. Wollborn J, Schuler A, Sheu RD, Shook DC, Nyman CB. Real-time multiplanar reconstruction imaging using 3-dimensional transesophageal echocardiography in structural heart interventions. J Cardiothorac Vasc Anesth. 2023;37:570-81.
11. Lemaire G, Vancraeynest D. Echocardiography of the aortic root: a practical approach for aortic valve-sparing surgery. Ann Cardiothorac Surg. 2023;12:194-212.
12. Papadopoulos K, Ikonomidis I, Coisne A, et al. Initial experience with the 4D mini-TEE probe in the adult population. J Clin Med. 2024;13:6450.
13. Iung B, Delgado V, Rosenhek R, et al. EORP VHD II Investigators. Contemporary presentation and management of valvular heart disease: the EURObservational Research programme valvular heart disease II survey. Circulation. 2019;140:1156-69.
14. Baumgartner H, Hung J, Bermejo J, et al. Recommendations on the echocardiographic assessment of aortic valve stenosis: a focused update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur Heart J Cardiovasc Imaging. 2017;18:254-75.
15. Otto CM. Valvular aortic stenosis: disease severity and timing of intervention. J Am Coll Cardiol. 2006;47:2141-51.
16. Nishi T, Shibayama K, Tabata M, et al. Accuracy and usefulness of aortic annular measurement using real-time three-dimensional transesophageal echocardiography: comparison with direct surgical sizing. J Cardiol. 2018;71:230-6.
17. Dima CN, Gaspar M, Mornos C, et al. Three-dimensional transesophageal echocardiography as an alternative to multidetector computed tomography in aortic annular diameter measurements for transcatheter aortic valve implantation. Biology. 2021;10:132.
18. Bleakley C, Eskandari M, Monaghan M. 3D transoesophageal echocardiography in the TAVI sizing arena: should we do it and how do we do it? Echo Res Pract. 2017;4:R21-32.
19. Mehrotra P, Flynn AW, Jansen K, et al. Differential left ventricular outflow tract remodeling and dynamics in aortic stenosis. J Am Soc Echocardiogr. 2015;28:1259-66.
20. Nanditha S, Malik V. Comparison of flow-independent parameters for grading severity of aortic stenosis using intraoperative transesophageal echocardiography - a prospective observational study. Ann Card Anaesth. 2020;23:425-8.
21. Gaspar T, Adawi S, Sachner R, et al. Three-dimensional imaging of the left ventricular outflow tract: impact on aortic valve area estimation by the continuity equation. J Am Soc Echocardiogr. 2012;25:749-57.
22. Saitoh T, Shiota M, Izumo M, et al. Comparison of left ventricular outflow geometry and aortic valve area in patients with aortic stenosis by 2-dimensional versus 3-dimensional echocardiography. Am J Cardiol. 2012;109:1626-31.
23. Kapadia SR, Leon MB, Makkar RR, et al. PARTNER trial investigators. 5-year outcomes of transcatheter aortic valve replacement compared with standard treatment for patients with inoperable aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet. 2015;385:2485-91.
24. Leon MB, Smith CR, Mack MJ, et al. PARTNER 2 Investigators. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2016;374:1609-20.
25. Mack MJ, Leon MB, Thourani VH, et al. PARTNER 3 Investigators. Transcatheter aortic-valve replacement in low-risk patients at five years. N Engl J Med. 2023;389:1949-60.
26. Forrest JK, Yakubov SJ, Deeb GM, et al. Low Risk Trial Investigators. 5-year outcomes after transcatheter or surgical aortic valve replacement in low-risk patients with aortic stenosis. J Am Coll Cardiol. 2025;85:1523-32.
27. Vahanian A, Beyersdorf F, Praz F, et al. ESC/EACTS Scientific Document Group. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2022;43:561-632.
28. Hayashida K, Bouvier E, Lefèvre T, et al. Impact of CT-guided valve sizing on post-procedural aortic regurgitation in transcatheter aortic valve implantation. EuroIntervention. 2012;8:546-55.
29. Lehmkuhl L, Foldyna B, Von Aspern K, et al. Inter-individual variance and cardiac cycle dependency of aortic root dimensions and shape as assessed by ECG-gated multi-slice computed tomography in patients with severe aortic stenosis prior to transcatheter aortic valve implantation: is it crucial for correct sizing? Int J Cardiovasc Imaging. 2013;29:693-703.
30. Rong LQ, Hameed I, Salemi A, et al. Three-dimensional echocardiography for transcatheter aortic valve replacement sizing: a systematic review and meta-analysis. J Am Heart Assoc. 2019;8:e013463.
31. Smith LA, Dworakowski R, Bhan A, et al. Real-time three-dimensional transesophageal echocardiography adds value to transcatheter aortic valve implantation. J Am Soc Echocardiogr. 2013;26:359-69.
32. Blanke P, Willson AB, Webb JG, et al. Oversizing in transcatheter aortic valve replacement, a commonly used term but a poorly understood one: dependency on definition and geometrical measurements. J Cardiovasc Comput Tomogr. 2014;8:67-76.
33. Akinseye OA, Jha SK, Ibebuogu UN. Clinical outcomes of coronary occlusion following transcatheter aortic valve replacement: a systematic review. Cardiovasc Revasc Med. 2018;19:229-36.
34. Mauri V, Frohn T, Deuschl F, et al. Impact of device landing zone calcification patterns on paravalvular regurgitation after transcatheter aortic valve replacement with different next-generation devices. Open Heart. 2020;7:e001164.
35. Hassan M, Abdrabou MM, Wahba WA, Samaan AA, Baghdady Y, Elamragy AA. Agreement between 4D transesophageal echocardiography and multi-detector computed tomography in measuring aortic root dimensions and coronary ostia heights. Int J Cardiovasc Imaging. 2023;39:1561-9.
36. de Agustin JA, Pozo Osinalde E, Olmos C, et al. Current usefulness of transesophageal echocardiography in patients undergoing transcatheter aortic valve replacement. J Clin Med. 2023;12:7748.
37. Shibayama K, Mihara H, Jilaihawi H, et al. 3D assessment of features associated with transvalvular aortic regurgitation after TAVR: a real-time 3D TEE study. JACC Cardiovasc Imaging. 2016;9:114-23.
38. Khalique OK, Hamid NB, White JM, et al. Impact of methodologic differences in three-dimensional echocardiographic measurements of the aortic annulus compared with computed tomographic angiography before transcatheter aortic valve replacement. J Am Soc Echocardiogr. 2017;30:414-21.
39. Kato N, Shibayama K, Noguchi M, et al. Superiority of novel automated assessment of aortic annulus by intraoperative three-dimensional transesophageal echocardiography in patients with severe aortic stenosis: Comparison with conventional cross-sectional assessment. J Cardiol. 2018;72:321-7.
40. Dumesnil JG, Pibarot P. Prosthesis-patient mismatch: an update. Curr Cardiol Rep. 2011;13:250-7.
41. Head SJ, Mokhles MM, Osnabrugge RLJ, et al. The impact of prosthesis-patient mismatch on long-term survival after aortic valve replacement: a systematic review and meta-analysis of 34 observational studies comprising 27 186 patients with 133 141 patient-years. Eur Heart J. 2012;33:1518-29.
42. Lancellotti P, Pibarot P, Chambers J, et al. Recommendations for the imaging assessment of prosthetic heart valves: a report from the European Association of Cardiovascular Imaging endorsed by the Chinese Society of Echocardiography, the Inter-American Society of Echocardiography, and the Brazilian Department of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2016;17:589-90.
43. Zoghbi WA, Jone PN, Chamsi-Pasha MA, et al. Guidelines for the evaluation of prosthetic valve function with cardiovascular imaging: a report from the American Society of echocardiography developed in collaboration with the society for Cardiovascular Magnetic Resonance and the Society of Cardiovascular Computed Tomography. J Am Soc Echocardiogr. 2024;37:2-63.
44. Pibarot P, Weissman NJ, Stewart J, et al. Incidence and sequelae of prosthesis-patient mismatch in transcatheter versus surgical valve replacement in high-risk patients with severe aortic stenosis: a PARTNER trial cohort-a analysis. J Am Coll Cardiol. 2014;64:1323-34.
45. ISO. International Standard, ISO 5840:2015. Cardiovascular implants-cardiac valve prostheses. International Organization for Standardization (ISO), 2015. Available from: https://www.iso.org/standard/77033.html#lifecycle [Last accessed on 19 Aug 2025].
46. Durko AP, Head SJ, Pibarot P, et al. Characteristics of surgical prosthetic heart valves and problems around labelling: a document from the European Association for Cardio-Thoracic Surgery (EACTS)-The Society of Thoracic Surgeons (STS)-American Association for Thoracic Surgery (AATS) valve labelling task force. Eur J Cardiothorac Surg. 2019;55:1025-36.
47. Mazzolai L, Teixido-Tura G, Lanzi S, et al. ESC Scientific Document Group. 2024 ESC Guidelines for the management of peripheral arterial and aortic diseases. Eur Heart J. 2024;45:3538-700.
48. Michelena HI, Della Corte A, Evangelista A, et al. Endorsed by the Heart Valve Society (HVS); European Association of Cardiovascular Imaging (EACVI); Society of Thoracic Surgeons (STS); American Association for Thoracic Surgery (AATS); Society for Cardiovascular Magnetic Resonance (SCMR); Society of Cardiovascular Computed Tomography (SCCT); North American Society for Cardiovascular Imaging (NASCI) and the International Bicuspid Aortic Valve Consortium (BAVCon). International consensus statement on nomenclature and classification of the congenital bicuspid aortic valve and its aortopathy, for clinical, surgical, interventional and research purposes. Eur J Cardiothorac Surg. 2021;60:448-76.
49. Paulis R, Salica A. Surgical anatomy of the aortic valve and root-implications for valve repair. Ann Cardiothorac Surg. 2019;8:313-21.
50. Malas T, Saczkowski R, Sohmer B, et al. Is aortic valve repair reproducible? Can J Cardiol. 2015;31:1497.e15-22.
51. Berrebi A, Monin JL, Lansac E. Systematic echocardiographic assessment of aortic regurgitation-what should the surgeon know for aortic valve repair? Ann Cardiothorac Surg. 2019;8:331-41.
52. Lang RM, Addetia K, Narang A, Mor-Avi V. 3-dimensional echocardiography: latest developments and future directions. JACC Cardiovasc Imaging. 2018;11:1854-78.
53. Hahn RT, Abraham T, Adams MS, et al. Guidelines for performing a comprehensive transesophageal echocardiographic examination: recommendations from the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013;26:921-64.
54. Smer A, Urja P, Anugula D, et al. Three-dimensional echocardiographic assessment of the aortic valve and the aorta. Echocardiography. 2022;39:1011-27.
55. Boodhwani M, de Kerchove L, Watremez C, et al. Assessment and repair of aortic valve cusp prolapse: implications for valve-sparing procedures. J Thorac Cardiovasc Surg. 2011;141:917-25.
56. Zoghbi WA, Adams D, Bonow RO, et al. Recommendations for noninvasive evaluation of native valvular regurgitation: a report from the american society of echocardiography developed in collaboration with the society for cardiovascular magnetic resonance. J Am Soc Echocardiogr. 2017;30:303-71.
57. Ranard LS, Bonow RO, Nishimura R, et al. Heart Valve Collaboratory. Imaging methods for evaluation of chronic aortic regurgitation in adults: JACC state-of-the-art review. J Am Coll Cardiol. 2023;82:1953-66.
58. Agricola E, Badano L, Mele D, et al. Real-time three dimensional transesophageal echocardiography: technical aspects and clinical applications. Heart Int. 2010;5:e6.
59. Stoebe S, Metze M, Jurisch D, et al. Analysis of chronic aortic regurgitation by 2D and 3D echocardiography and cardiac MRI. Echo Res Pract. 2018;5:51-62.
60. Ewe SH, Delgado V, van der Geest R, et al. Accuracy of three-dimensional versus two-dimensional echocardiography for quantification of aortic regurgitation and validation by three-dimensional three-directional velocity-encoded magnetic resonance imaging. Am J Cardiol. 2013;112:560-6.
61. Choi J, Hong GR, Kim M, et al. Automatic quantification of aortic regurgitation using 3D full volume color doppler echocardiography: a validation study with cardiac magnetic resonance imaging. Int J Cardiovasc Imaging. 2015;31:1379-89.
62. Shanks M, Siebelink HM, Delgado V, et al. Quantitative assessment of mitral regurgitation: comparison between three-dimensional transesophageal echocardiography and magnetic resonance imaging. Circ Cardiovasc Imaging. 2010;3:694-700.
64. Connor B, Takei M, Clark DE, Maskatia SA. Improved quantification of aortic regurgitation with direct regurgitant jet measurement by four-dimensional flow cardiovascular magnetic resonance in complex congenital heart disease. J Cardiovasc Magn Reson. 2025;27:101876.
65. Belli M, Margonato D, Prandi FR, et al. Diagnosis of atrial cardiomyopathy: from the electrocardiogram to the new opportunities with multimodality imaging. J Cardiovasc Med. 2025;26:88-101.
66. Schäfers HJ, Schmied W, Marom G, Aicher D. Cusp height in aortic valves. J Thorac Cardiovasc Surg. 2013;146:269-74.
67. Schäfers HJ, Bierbach B, Aicher D. A new approach to the assessment of aortic cusp geometry. J Thorac Cardiovasc Surg. 2006;132:436-8.
68. Schäfers HJ, Aicher D, Langer F, Lausberg HF. Preservation of the bicuspid aortic valve. Ann Thorac Surg. 2007;83:S740-5; discussion S785.
70. De Paulis R, Chirichilli I, De Kerchove L, et al. Current status of aortic valve repair surgery. Eur Heart J. 2025;46:1394-411.
71. Ehrlich T, de Kerchove L, Vojacek J, et al. State-of-the art bicuspid aortic valve repair in 2020. Prog Cardiovasc Dis. 2020;63:457-64.
72. Rodríguez-Palomares JF, Dux-Santoy L, Guala A, Galian-Gay L, Evangelista A. Mechanisms of aortic dilation in patients with bicuspid aortic valve: JACC state-of-the-art review. J Am Coll Cardiol. 2023;82:448-64.
73. La Mura L, Lembo M, Musella F, et al. Aortic regurgitation in bicuspid aortic valve: the role of multimodality imaging. J Clin Med. 2024;13:3924.
74. Italiano G, Tamborini G, Fusini L, et al. Feasibility and accuracy of the automated software for dynamic quantification of left ventricular and atrial volumes and function in a large unselected population. J Clin Med. 2021;10:5030.
75. Marigliano AN, Ortiz JT, Casas J, Evangelista A. Aortic regurgitation: from valvular to myocardial dysfunction. J Clin Med. 2024;13:2929.
76. Tretter JT, Burbano-Vera NH, Najm HK. Multi-modality imaging evaluation and pre-surgical planning for aortic valve-sparing operations in patients with aortic root aneurysm. Ann Cardiothorac Surg. 2023;12:295-317.
77. Hahn RT, Leipsic J, Douglas PS, et al. Comprehensive echocardiographic assessment of normal transcatheter valve function. JACC Cardiovasc Imaging. 2019;12:25-34.
Cite This Article
How to Cite
Download Citation
Export Citation File:
Type of Import
Tips on Downloading Citation
Citation Manager File Format
Type of Import
Direct Import: When the Direct Import option is selected (the default state), a dialogue box will give you the option to Save or Open the downloaded citation data. Choosing Open will either launch your citation manager or give you a choice of applications with which to use the metadata. The Save option saves the file locally for later use.
Indirect Import: When the Indirect Import option is selected, the metadata is displayed and may be copied and pasted as needed.
About This Article
Special Issue
Copyright
Data & Comments
Data

















Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.