Squamous cell carcinoma of the upper urinary tract in patients with urolithiasis: a systematic review
Abstract
Aim: To perform a systematic review on the current evidence about the squamous cell carcinoma (SCC) of the upper urinary tract in patients with urolithiasis.
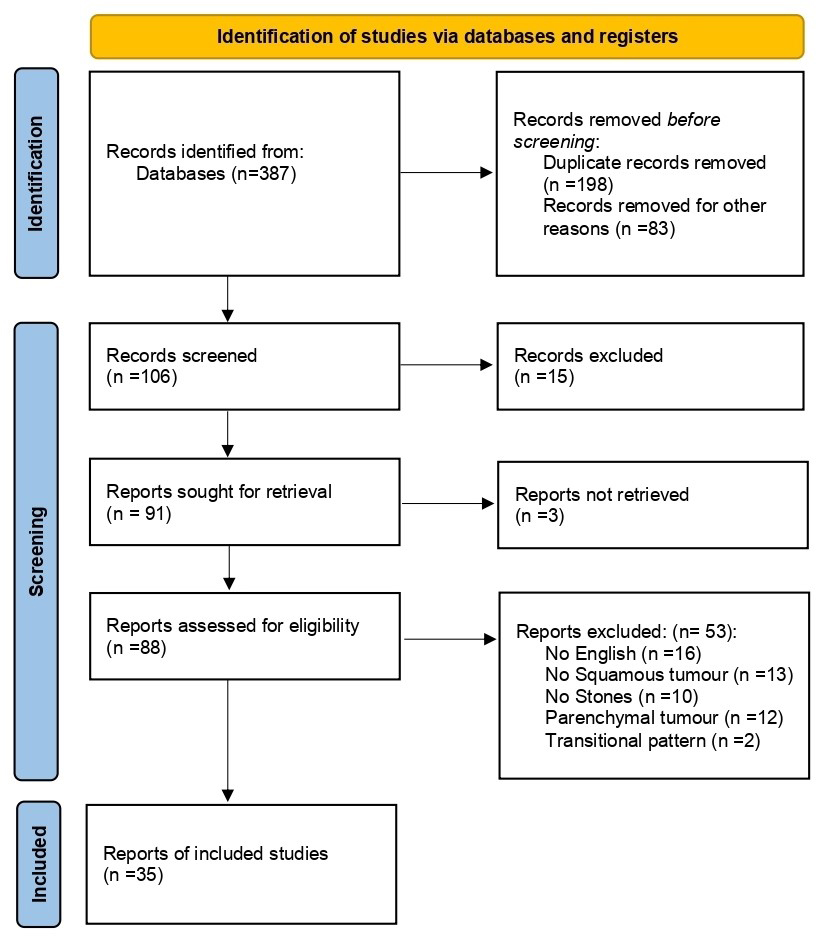
Methods: A comprehensive bibliographic search on the MEDLINE, Scopus, Web of Science, and Cochrane Library databases was performed in December 2024. The SPIDER (Sample, Phenomenon of Interest, Design, Evaluation, Research type) framework was used to define inclusion criteria: male and female patients with urolithiasis (S); presence of SCC of the upper urinary tract (PI); prospective and retrospective studies (D); diagnosis based on imaging or pathological examination (E); qualitative, quantitative or mixed-methods (R). Quality of studies was assessed with Murad scale. Extracted data were synthesized in a narrative fashion. PROSPERO ID: “CRD42024625816”.
Results: A total of 35 articles were included. Eight case series (22.9%) and 27 case reports (77.1%) were analyzed. The overall quality of papers was low. Sixty-three cases of SCC in patients with urolithiasis (range: 1-11) were identified. The male-to-female ratio was 1.55, with a median age of 60 years (range: 25-87). Most common symptoms included pain (70%), hematuria (60%), and infection (40%). Staghorn stones (48%) and multiple stones (42%) were the most frequently encountered types of calculi. Almost all SCCs (97%) developed in the calico-pyelic system. A radiological suspicion of SCC was raised using imaging in 64% of patients, while in 52% of cases it was an incidental finding during pathological examination after nephrectomy for a non-functional kidney. Locally advanced disease was observed in 44% of patients, while metastasis was reported in 16%. The overall prognosis was poor, with a survival of approximately 6 months and 1-2 years for metastatic and locally advanced cases, respectively.
Conclusion: The available evidence is poor because the disease is extremely rare and the literature is limited to isolated case reports and small series. Therefore, robust conclusions cannot be drawn. Only a limited number of cases are reported in the literature and the current data prevent the estimation of prevalence or reliable pathophysiologic hypotheses. However, this tumor appears to be associated with a severe prognosis. Further investigations are needed to explore the topic and provide sufficient evidence to formulate clear recommendations.
Keywords
INTRODUCTION
Upper tract urothelial carcinoma (UTUC) is a malignant neoplasm arising from the urothelium of the upper urinary tract, accounting for approximately 5%-10% of all urothelial carcinoma cases, with an estimated prevalence of two cases per 100,000 inhabitants[1]. These tumors are relatively uncommon yet highly malignant, originating from urothelial cells lining the renal calyces, renal pelvis, and ureters. While most upper urinary tract tumors are of the urothelial type, histological variants occur in up to 25% of cases[2], each with distinct risk factors and epidemiological profiles that differ significantly from those of conventional bladder cancer[3,4].
Among these histological variants, squamous cell carcinoma (SCC) of the upper urinary tract is particularly rare, accounting for only a small fraction of cases. Despite its low incidence, SCC seems to be associated with increased aggressiveness, significant diagnostic and therapeutic challenges, and overall poor prognosis[4].
Some evidence suggests that SCC pathogenesis could be linked to chronic inflammation of the urinary tract epithelium. This process would initially induce squamous metaplasia of the urothelium, which may subsequently undergo malignant transformation into SCC. It has been hypothesized that, in the upper urinary tract, the primary etiological factor implicated in this transformation could be the presence of stones. In particular, long-standing untreated stone disease is believed to sustain chronic inflammation, providing a pathological substrate for the malignant transformation of the urothelium[5,6].
Imaging findings of renal SCC range from solid renal masses to hydronephrosis, calcifications, and regional lymphadenopathy. However, these features are largely nonspecific, making it challenging to differentiate SCC from chronic inflammatory conditions such as xanthogranulomatous pyelonephritis or renal tuberculosis[3,7].
Due to its rarity, SCC of the upper urinary tract remains poorly documented. Indeed, most available evidence derives from case reports and small case series, and topic-specific guidelines are lacking. Consequently, further research is essential to improve the understanding of this malignancy and optimize its management[8].
The primary aim of this systematic review is to provide a comprehensive analysis of the current scientific evidence on SCC of the upper urinary tract in patients with renal and ureteral stone disease.
MATERIALS AND METHODS
Search strategy
A comprehensive bibliographic search was conducted in December 2024 using the MEDLINE, Scopus, Web of Science, and Cochrane Library databases to identify studies investigating the current evidence on SCC of the upper urinary tract in patients with urolithiasis. Different combinations of the following keywords were used in a title/abstract search, applying Boolean operators: kidney, renal, pelvis, calyx, ureter, upper, urinary tract, UTUC, stone, calculi, lithiasis, urolithiasis, squamous, tumor, neoplasia, carcinoma. Additionally, the reference lists of retrieved articles were manually screened to identify further relevant studies. The literature search was restricted to English-language articles and studies on human subjects. No restrictions were applied regarding the publication date.
Study selection
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines[9]. The SPIDER (Sample, Phenomenon of Interest, Design, Evaluation, Research type)[10] framework was used to define the inclusion criteria.
(1) Sample (S): Male and female patients with urolithiasis;
(2) Phenomenon of Interest (PI): Presence of SCC of the upper urinary tract;
(3) Design (D): Prospective and retrospective studies (including case series and case reports);
(4) Evaluation (E): Diagnosis based on imaging or pathological examination;
(5) Research type (R): Qualitative, quantitative, or mixed-methods studies.
A two-step screening process was implemented. Initially, titles and abstracts were reviewed to identify potentially relevant studies. Full-text articles that met the inclusion criteria underwent a detailed assessment to confirm eligibility.
Data extraction
The following data points were extracted from each included study: first author, publication year, country of origin, number of patients, age, sex, symptoms, stone characteristics, site of tumor, presence of hydronephrosis, radiological diagnosis of tumor, incidental diagnosis of tumor, microscopic findings, pathological stage, treatment of tumor, follow-up, and prognosis.
Quality assessment
The level of evidence (LoE) was evaluated according to the Oxford Center for Evidence-Based Medicine 2011[11]. Study quality was assessed using the Murad scale[12] and arbitrarily categorized according to the total score as follows:
(1) Low quality: 0-3 points;
(2) Intermediate quality: 4-5 points;
(3) High quality: 6-8 points.
Data analysis and synthesis
Due to the expected paucity, low quality, and heterogeneity of the available data, we decided not to perform a meta-analysis. Consequently, the results were reported in a narrative fashion. In particular, the extracted data were presented in the text and tables as shown in the original articles. However, when deemed necessary for a better overview, they were combined into sums, percentages, ranges, and medians.
Other methodological details
The review methods were established before the study began, and the protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) under the ID “CRD42024625816”. Study selection, data extraction, and quality assessment were performed independently by two authors (MS, ST), while a third author (CM) resolved any disagreements.
RESULTS
A total of 35 articles were included in this review, comprising 8 case series (22.9%) and 27 case reports (77.1%) [Figure 1 and Table 1]. The studies collectively analyzed 63 patients, with a male-to-female ratio of 1.55 and a median age of 60 years (range: 25-87).
Main characteristics of the included studies
| First author, Publication year | Country of origin | Study design | Number of patients | Level of Evidence* | Quality of study** |
| Sözer, 1968[13] | Turkey | Case report | 1 | 4 | 1 |
| Leong et al., 1976[14] | China | Case series | 3 | 4 | 2 |
| Kinn, 1975[15] | Sweden | Case series | 6 | 4 | 2 |
| Howat et al., 1983[16] | England | Case report | 1 | 4 | 2 |
| Li and Cheung 1987[17] | China | Case series | 11 | 4 | 4 |
| Mhiri et al., 1989[18] | Tunisia | Case series | 3 | 4 | 4 |
| Narumi et al., 1989[19] | Japan | Case series | 4 | 4 | 3 |
| Sheaff et al., 1996[20] | England | Case report | 1 | 4 | 3 |
| Kimura et al., 2000[21] | Japan | Case report | 1 | 4 | 1 |
| Kim et al., 2001[22] | Korea | Case report | 1 | 4 | 2 |
| Sivaramakrishna et al., 2004[23] | India | Case report | 1 | 4 | 3 |
| Ham et al., 2011[24] | Korea | Case report | 1 | 4 | 3 |
| Jain et al., 2011[4] | India | Case series | 4 | 4 | 3 |
| Verma et al., 2011[25] | India | Case report | 1 | 4 | 3 |
| Paonessa et al., 2011[26] | USA | Case report | 1 | 4 | 2 |
| Bhaijee, 2012[3] | USA | Case report | 1 | 4 | 3 |
| Di Battista et al., 2012[27] | Italy | Case report | 1 | 4 | 3 |
| Kalayci et al., 2013[28] | Turkey | Case report | 1 | 4 | 3 |
| Jongyotha and Sriphrapradang, 2015[29] | Thailand | Case report | 1 | 4 | 4 |
| Xiao et al., 2015[30] | China | Case series | 2 | 4 | 1 |
| Nachiappan et al., 2016[31] | India | Case report | 1 | 4 | 2 |
| Jakes et al., 2016[32] | UK | Case report | 1 | 4 | 2 |
| Hassan and Qureshi, 2017[7] | Pakistan | Case report | 1 | 4 | 3 |
| Deng et al., 2017[33] | China | Case report | 1 | 4 | 6 |
| Kartal et al., 2019[34] | Turkey | Case report | 1 | 4 | 1 |
| Sun and Li, 2020[35] | China | Case report | 1 | 4 | 1 |
| Hosseinzadeh and Mohammadzadeh, 2020[36] | Iran | Case report | 1 | 4 | 5 |
| Chaurasia, 2021[37] | India | Case report | 1 | 4 | 3 |
| Terakawa et al., 2021[38] | Japan | Case report | 1 | 4 | 3 |
| Oh and Kim, 2022[39] | Republic of Korea | Case report | 1 | 4 | 3 |
| Liu et al., 2022[40] | China | Case report | 1 | 4 | 2 |
| Patel et al., 2023[41] | India | Case series | 4 | 4 | 2 |
| Priyatharsan et al., 2023[42] | Sri Lanka | Case report | 1 | 4 | 3 |
| Alnefaie et al., 2024[43] | SAU | Case report | 1 | 4 | 2 |
| Qiao et al., 2024[44] | China | Case report | 1 | 4 | 5 |
Quality assessment
The methodological quality of the included studies was generally low. All studies corresponded to a Level of Evidence 4, reflecting the retrospective design and the predominance of case reports and small case series. According to the Murad scale, 29 studies (82.8%) were classified as low quality (score 0–3), 5 (14.3%) as intermediate quality (score 4–5), and only 1 (2.8%) as high quality (score ≥6). These findings highlight the limited robustness of the available evidence and the considerable risk of bias, which must be considered when interpreting the clinical and prognostic outcomes of this review.
Among the 8 case series, a total of 36 patients were identified. Sex was reported for 29 patients, of whom 17 were male (59%) and 12 were female (41%). The most frequently reported symptoms included pain (81%), hematuria (30%), and infection (51%). Regarding stone characteristics, staghorn calculi (62%) and multiple calculi (19%) were the most common types. Table 2 summarizes data from case series.
Main findings of included case series
| Reference | Age | N | Sex | Symptoms | Stone characteristics | Hydronephrosis | Site of SCC | Radiological diagnosis of SCC | Incidental diagnosis of SCC | Microscopic findings | Pathological stage | Treatment of SCC | Last Follow-up and prognosis |
| Leong et al., 1976[14] | 56* | 3 | NA | Hematuria, mass, infection | NA | Yes | Upper calix | No | Yes | SCC | Metastatic | Nephrectomy | Death at: -13m DOD -1m DOC -1m DOC |
| Kinn, 1975[15] | 45* 60 | 6** | 1M 1F | Fever, hematuria, Infection, fistula, pain | Staghorn | Yes | RP | 1 Yes 1 No | 1 Yes 1 No | Poorly differentiated SCC | NA | Nephrectomy | Death at: -1y DOC -3m DOC -2m DOD |
| Li and Cheung 1987[17] | 60 69 73 69 45 62 43 60 67 65 45 | 11 | 5M 6F | Pain, mass, infection | Staghorn | Yes | RP | 3 Yes | 8 Yes | SCC | 8 TxN+ 3 M1 | Nephrectomy Nephroureterectomy, CT/RT | Death at: -3w -72m -2m -4m -1m -2w -7m -1m -5m -5m -1w |
| Mhiri et al., 1989[18] | 57 47 | 2 | 2M | Pain, infection Pain, fever, mass | Staghorn in horseshoe kidney | Yes | RP RP | No | Yes | SCC | NA | Nephrectomy | -Death at 7m DOD -Death at 8m DOD |
| Narumi et al., 1989[19] | 54 61 63 79 | 4 | 3M 1F | Pain, hematuria | NA | NA | 2 Ureter 2 RP | 4 Yes | No | SCC | <pT2N0 pT4N0 pT3N0 pT3N0 | Nephrectomy | NA |
| Jain et al., 2011[4] | 50 87 50 53 | 4 | 3M 1F | Pain, mass | Staghorn stones | Yes | RP | 1 Yes | 3 Yes | Well differentiated SCC 1 Poorly differentiated SCC | pT2N0M0 pT3N2cM0 pT3pN0Mx pT3N0M0 | Nephrectomy + 2 CT | -NA -DOC -Alive a 3m NED -Alive at 5 m NED |
| Xiao et al., 2015[30] | 55 61 | 2 | 1F, 1M | Pain, mass, hematuria | Multiple stones, bilateral | Yes | RP | 2 Yes | No | Well differentiated SCC | T3N0M0 T3N0M0 | Radical nephrectomy | -Death at 12m DOC -DOD |
| Patel et al., 2023[41] | 61 25 79 77 | 4 | 2F, 2M | Pain, weight loss | Multiple stones | Yes | RP | 3 No 1 Yes | 3 Yes 1 No | SCC | T1bN0Mx T1bN0Mx T2N0M0 T3N0Mx | 3 Nephrectomy 1 Radical nephrectomy | NA |
Among the 27 case reports, 17 men (63%) and 10 women (37%) were detected. The most commonly reported symptoms were pain (74.1%), hematuria (22%), and infection (22%). The most frequent types of stones were staghorn calculi (40.7%) and multiple calculi (29.6%). Table 3 presents findings from case reports.
Main findings of included case reports
| Reference | Age | Sex | Symptoms | Stone characteristics | Hydronephrosis | Site of SCC | Radiological diagnosis of SCC | Incidental diagnosis of SCC | Microscopic findings | Pathological stage | Treatment of SCC | Last Follow-up and prognosis |
| Sözer, 1968[13] | 46 | F | Pyuria, hematuria | Multiple stones | Na | Ureter | No | Yes | SCC | NA | Ureterectomy, RT | NA |
| Leong et al., 1976[14] | 35 | F | Pain, hematuria, infection | Staghorn stone | Yes | RP | No | Yes | Well differentiated SCC | pTxN+ | Laparotomy, RT | Death at 4m |
| Sheaff et al., 1996[20] | 41 | M | Pain, fever | Stone in horseshoe kidney | Na | RP | No | Yes | Verrucous form of Well differentiated SCC | NA | Partial nephrectomy | Alive at 6m NED |
| Kimura et al., 2000[21] | 48 | M | Mass, hematuria | Staghorn stone | Yes | RP | Yes | No | SCC | M1 | Biopsy + CT | Death at 1m DOD |
| Kim et al., 2001[22] | 60 | M | Pain, mass | Ureteral stone | Yes | RP, Ureter | No | Yes | SCC | NA | Nephroureterectomy | Alive at 36m NED |
| Sivaramakrishna et al., 2004[23] | 46 | M | Pain, fever, hematuria | Large renal stone | Yes | RP | Yes | No | SCC | NA | Nephroureterectomy, radiotherapy | Alive at 12m NED |
| Verma et al., 2011[25] | 62 | M | Pain, mass, fever | Multiple stones | Yes | RP | No | Yes | SCC | NA | Nephrectomy, CT | NA |
| Paonessa et al., 2011[26] | 70 | F | Pain | Multiple stones | No | RP | Yes | No | Poorly differentiated SCC | pT1-2 | Nephrectomy | NA |
| Ham et al., 2011[24] | 69 | M | Pain, mass, weight loss | Multiple stones | Yes | RP | No | Yes | Poorly differentiated SCC | pT3N0M0 | Nephrectomy | Death at 7m DOD |
| Bhaijee, 2012[3] | 77 | F | Weight loss, anemia | Staghorn stone | Yes | RP | Yes | No | SCC in situ | pT3 | Nephrectomy | Alive at 6m NED |
| Di Battista et al., 2012[27] | 50 | M | Hematuria, fever, mass | Multiple stones | Yes | RP | Yes | No | SCC | M1 | Biopsy, RAE, CT | Death at 1m |
| Kalayci et al., 2013[28] | 63 | M | Weight loss, | Staghorn stones | Yes | RP, upper calix | Yes | No | Poorly differentiated SCC | pT3N0M0 | Nephrectomy | NA |
| Jongyotha and Sriphrapradang, 2015[29] | 79 | F | Weight loss, low mental status, pain | Staghorn stones | Yes | RP | Yes | No | SCC | M1 | Biopsy + palliative care | Death at 1m |
| Nachiappan et al., 2016[31] | 60 | F | Pain, fever, infection | Staghorn stones | Yes | RP | Yes | No | SCC | PTx N0 | Nephrectomy | NA |
| Jakes et al., 2016[32] | 46 | M | Pyuria, infection | Bilateral stones | No | RP | Yes | No | Well differentiated SCC | NA | Nephrectomy | NA |
| Hassan and Qureshi, 2017[7] | 45 | M | Pain, infection | Multiple stones, impacted | Yes | RP | No | Yes | Mod differentiated SCC | pT3 Nx | Nephrectomy | NA |
| Deng et al., 2017[33] | 61 | M | Pain | Large stone | Yes | RP | Yes | No | Well differentiated SCC | pTxN+ | Nephrectomy | Alive at 6m NED |
| Kartal et al., 2019[34] | 38 | F | Pain | Staghorn stones | Yes | RP | Yes | No | SCC | M1 | Nephrectomy, CT | Death at 17m |
| Sun and Li, 2020[35] | 66 | M | Pain, mass, ulcer | Large stone | Yes | RP | No | Yes | Mod differentiated SCC | M1 | Nephrectomy, RT | Death at 3m |
| Mohammadzadeh, 2020[36] | 59 | F | Pain, hematuria | Staghorn stones | Yes | RP | Yes | No | Well differentiated SCC | pT3 | Radical nephrectomy | Death 12m DOD |
| Chaurasia, 2021[37] | 43 | M | Pain | Multiple stones | Yes | RP | No | Yes | SCC | pT3NxMx | Nephrectomy | Alive at 12m |
| Terakawa et al., 2021[38] | 74 | F | Pain, malaise | Large, stone, ADPKD | No | RP | Yes | No | Well differentiated SCC | pT1-3 | Nephrectomy, ileocecal resection | Death at 2m DOC |
| Oh and Kim, 2022[39] | 61 | M | Pain | Staghorn stones | Yes | RP | Yes | No | Well differentiated SCC | pT4N0 | Radical nephrectomy, hemicolectomy, LND | Alive at 6m |
| Liu et al., 2022[40] | 54 | F | Pain, mass | 8mm stone | Yes | RP | Yes | No | SCC differentiated | NA | Radical nephrectomy, CT | Death at 7m DOD |
| Priyatharsan et al., 2023[42] | 72 | M | Pain, fever, weight loss | Staghorn stones | Yes | RP | Yes | No | SCC | pT4 | Biopsy, palliative RT | NA |
| Alnefaie et al., 2024[43] | 60 | M | Pain, nausea, | Staghorn stones | Yes | RP | No | Yes | SCC | M1 | Nephrectomy, fistula repair | NA |
| Qiao et al., 2024[44] | 59 | M | Infection | Multiple stones | Yes | RP | NA | NA | SCC | NA | RAE | NA |
Almost all SCCs (97%) developed in the calyceal-pelvic system. Hydronephrosis was observed in 54 patients (85.7%). A radiological suspicion of SCC was raised in 38% of cases, whereas in 44% it was incidentally detected during pathological examination after nephrectomy for a non-functional kidney.
Pathological findings
Histological evaluation confirmed that the majority of tumors were pure SCC; although occasional cases with mixed histology (verrucous components) were described, studies reporting transitional variants were excluded from the analysis. Tumor grade was variably reported, with poorly differentiated forms prevailing among advanced cases. Pathological staging, available in a subset of patients, showed that 40% of patients presented with advanced disease [mainly pathologic T3-T4 (pT3-pT4), and, when available, node-positive status (pN+)], while early-stage tumors (pT1-pT2) were rare and usually detected incidentally. Distant metastases were reported in 16% of cases. Lymph node involvement was inconsistently documented but, when present, was associated with adverse outcomes. Overall, advanced stage and poor differentiation correlated with long-standing staghorn calculi, hydronephrosis, and poor survival. Prognosis remained dismal, with a median survival of approximately 6 months in metastatic cases and 1–2 years in patients with locally advanced disease, whereas incidentally detected, well-differentiated tumors tended to show more favorable outcomes.
DISCUSSION
Summary of findings
The collected case series and case reports highlighted the rare yet aggressive nature of SCC of the upper urinary tract; all cases included in this review were reported in association with urolithiasis. Therefore, the actual incidence of this condition among SCC of the upper tract cannot be determined. Most of patients presented with hematuria, pain, or mass effect, and a strong correlation was observed between SCC and the presence of staghorn or multiple calculi. At diagnosis, the disease was often locally advanced or metastatic, leading to poor outcomes despite surgical intervention. Treatment primarily involved nephrectomy or radical nephroureterectomy, sometimes combined with chemotherapy or radiotherapy, although no standard systemic therapy had been established. Although the available data should be interpreted with caution, as they mainly derive from advanced-stage cases, they suggest that SCC of the upper urinary tract is characterized by a generally poor prognosis.
Pathophysiological mechanisms
The findings highlight a recurrent coexistence of stones and upper tract tumors, suggesting a potential relationship, although the strength of this association cannot be defined and the underlying mechanisms remain unclear. Several factors have been hypothesized to contribute to SCC development in the upper urinary tract.
(1) Mechanical Stimulation and Chronic Inflammation: persistent mechanical irritation from kidney stones led to chronic inflammation, which in turn promotes urothelial metaplasia, hyperplasia, and eventually malignant transformation[45-48].
(2) Cytokines and Oxidative Stress: chronic inflammation triggers the release of cytokines, chemokines, and free radicals, which promote cellular damage, uncontrolled proliferation, and tumor growth[49].
(3) Carcinogen Retention: urinary tract obstruction caused by stones may lead to prolonged exposure to potential carcinogens, accelerating tumor progression[39,41,44,50].
In summary, kidney stones contribute to an environment of chronic inflammation, oxidative stress, and carcinogen exposure, creating favorable conditions for malignant transformation of the urothelium. Further molecular investigations are required to clarify these mechanisms.
Studies have not been able to identify specific environmental or occupational risk factors due to the limited accuracy in reporting this information. Regarding epidemiology, slight predominance of males over females has been observed, and the median age at diagnosis was 60 years.
Our review has confirmed that SCC of the upper urinary tract predominantly originated in the renal pelvis, with only a small percentage (3%) of cases affecting the ureter. The lower occurrence in the ureter had suggested that differences in epithelial exposure to irritants or site-specific immune responses may influence carcinogenesis[4,30].
Additionally, SCC has been reported in kidneys with congenital or acquired abnormalities, including horseshoe kidney, ectopic kidney, polycystic kidney disease, and renal calyceal diverticula[51,52]. These findings suggested that structural anomalies may predispose certain individuals to chronic irritation and subsequent malignant transformation.
Clinical management
Direct comparison with conventional UTUC could not be performed, as no control group was included in this review. However, this differs from clinical practice and guideline recommendations, where conventional urothelial carcinoma of the upper tract is used as the standard reference for assessing the prognostic and therapeutic implications of distinct histological entities such as SCC.
The frequent coexistence of large calculi and chronic inflammation may lead to an initial misdiagnosis as chronic pyelonephritis[3,37]. Moreover, SCC often presents insidiously, with symptoms frequently overlapping with those of urolithiasis, including flank pain and hematuria. This nonspecific clinical picture makes early recognition difficult, often leading to a delayed diagnosis. Consequently, in most cases, SCC is detected incidentally following nephrectomy for a non-functioning kidney rather than through preoperative imaging findings[53,54].
In several studies[21,27,29,42,44], the diagnosis of SCC has been made through biopsies. Therefore, in cases of suspicious stone-related lesions observed during surgery, it is advisable to perform multiple histological biopsies.
Despite advances in imaging techniques, SCC remains challenging to detect radiologically. Ultrasound and computed tomography (CT) scans often fail to differentiate SCC from chronic inflammatory conditions, leading to misinterpretation or underestimation of the disease burden[19,28]. Although contrast-enhanced CT can provide valuable insights into tumor extent, its diagnostic accuracy remains limited, particularly in patients with chronic kidney disease who cannot undergo contrast studies. Furthermore, urine cytology has low sensitivity due to the presence of stones, which may prevent tumor cell shedding into the urinary tract or may cause confounding inflammatory changes in the exfoliated cells[44,55].
Given these diagnostic challenges, periodic imaging evaluations, particularly in patients with long-standing urolithiasis, hydronephrosis, or renal dysfunction, should be considered.
Therapeutic approaches remain non-standardized, with radical nephroureterectomy and lymph node dissection being the preferred surgical strategy. However, due to frequent late-stage presentation, surgery alone rarely improves long-term survival. Unlike urothelial carcinoma, where chemotherapy and immunotherapy have improved outcomes, no systemic therapies have been established for SCC. Although radiotherapy and chemotherapy have been attempted in select cases, their efficacy remains largely uncertain, underscoring the urgent need for further research into targeted therapies[17,46].
Prognosis
The prognosis of SCC of the upper urinary tract is markedly worse than that of urothelial carcinoma (UTUC), largely due to the frequent occurrence of delayed diagnosis, limited systemic treatment options, and the aggressive biological behavior of the tumor[4,39]. In our review, most patients were diagnosed at an advanced stage, with local invasion or distant metastases present in a significant proportion of cases (44% and 16%, respectively).
Where available, survival data revealed median overall survival (OS) ranging between 5 and 7 months in patients with metastatic disease, and 12 to 24 months in those with locally advanced but non-metastatic disease. Disease-free survival (DFS) was rarely reported in the literature, but isolated case reports indicated recurrence within 2 to 8 months after surgery in several patients with high-grade tumors.
Only a minority of patients - fewer than 10% - achieved survival beyond 5 years. Long-term survivors were more likely to have been diagnosed incidentally at an early stage and to have undergone radical surgery without evidence of lymphovascular invasion or metastasis at presentation[4,55].
Several potential prognostic factors were identified:
(1) Tumor stage at diagnosis: Strongly associated with survival, with metastatic cases faring worst.
(2) Histological grade: Particularly poorly differentiated tumors, correlated with shorter OS.
(3) Mode of diagnosis: Patients with incidentally discovered tumors following nephrectomy for presumed benign conditions had better outcomes than those diagnosed based on imaging.
(4) Stone burden: Presence of staghorn calculi and prolonged stone disease was frequently associated with delayed diagnosis and more advanced disease.
In contrast, UTUC generally has a more favorable prognosis when detected early, supported by the availability of standardized staging, risk stratification systems, and established systemic treatments including chemotherapy and immune checkpoint inhibitors.
These findings underscore the urgent need for earlier detection, consistent staging, and more effective systemic therapies in this patient population.
Strengths, limitations, and future directions
To the best of our knowledge, this is the first systematic review specifically investigating the association between upper urinary tract SCC and urolithiasis. It provides a comprehensive synthesis of the existing evidence and highlights recurring clinical and radiological patterns in a condition that remains poorly understood. This work offers a valuable reference point for clinicians and researchers confronted with this rare malignancy.
The main limitation of the available literature is the predominance of low-quality retrospective evidence, primarily composed of isolated case reports and small case series, which limits the generalizability of findings and hinders the development of evidence-based recommendations. Additionally, there is a lack of standardized reporting regarding imaging findings, pathological details, and follow-up outcomes across the included studies.
(1) Future research should focus on clearly defined and feasible objectives, including the establishment of multicenter registries or collaborative databases to systematically collect data on SCC cases in patients with urolithiasis;
(2) Prospective studies assessing the incidence of SCC in high-risk populations (e.g., those with long-standing staghorn stones or non-functioning kidneys);
(3) Implementation of standardized imaging protocols and diagnostic algorithms aimed at distinguishing SCC from chronic pyelonephritis or xanthogranulomatous pyelonephritis;
(4) Histopathologic and molecular profiling studies to identify biomarkers that may enable earlier diagnosis or serve as therapeutic targets;
(5) Clinical trials or retrospective cohort analyses evaluating the effectiveness of systemic treatments (e.g., chemotherapy, immunotherapy) in SCC of the upper tract, possibly adapted from urothelial carcinoma protocols.
Clarifying the pathophysiologic mechanisms linking chronic inflammation, urolithiasis, and malignant transformation of the urothelium will also be critical. A deeper mechanistic understanding could support the development of targeted preventive strategies, such as timely surgical treatment of high-risk stone disease and surveillance imaging in selected patients.
Ultimately, strengthening the quality of evidence through well-structured research will be essential to guide clinical decision-making and allow for the development of specific diagnostic and therapeutic guidelines.
In conclusion, SCC of the upper urinary tract is an exceptionally rare and aggressive malignancy, most frequently associated with chronic and complex urolithiasis. Its nonspecific clinical features and overlap with benign conditions often result in delayed or incidental diagnosis, which contributes to a generally poor prognosis. The current literature is limited to low-quality retrospective studies, mostly case reports and small series, which hinders the ability to draw definitive conclusions regarding epidemiology, pathogenesis, and optimal management. Furthermore, there is a lack of validated diagnostic algorithms and no standardized systemic therapies tailored to SCC of the upper urinary tract. Clinicians should maintain a high index of suspicion in patients with long-standing staghorn or infected stones, particularly in the setting of a non-functioning kidney. However, given the scarcity of robust evidence, caution is warranted in extrapolating management strategies from other urologic malignancies. Future research should prioritize prospective multicenter data collection, improved radiologic and histopathologic diagnostic protocols, and translational studies aimed at identifying molecular targets. High-quality studies are needed to clarify the natural history of the disease, define risk factors, and guide the development of evidence-based clinical guidelines.
DECLARATIONS
Authors’ contributions
Conceptualization: Stizzo M, Manfredi C
Study selection: Stizzo M; Tammaro S
Data extraction: Stizzo M, Tammaro S
Manuscript writing: Stizzo M, Tammaro S, Rubinacci A
Quality assessment: Stizzo M, Tammaro S, Arcaniolo D, Spirito L, Goumas IK, Giusti G, Puliatti S, Tailly T
Grammatical review: Manfredi C, Arcaniolo D, Spirito L, Goumas IK, Giusti G, Puliatti S, Tailly T
Scientific review: Arcaniolo D, Spirito L, Goumas IK, Giusti G, Puliatti S, Tailly T
Tables editing: Rubinacci A, De Sio M
Manuscript writing: Rubinacci A
Development of methodology: Manfredi C
Supervision: De Sio M
All authors made substantial contributions to the manuscript and approved its final version.
Availability of data and materials
All reported data are available in the selected articles. Raw results of the bibliographic search and study selection process are available upon justified request to the corresponding author.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2025.
REFERENCES
1. Gontero P, Birtle A, Capoun O, et al. European association of urology guidelines on non-muscle-invasive bladder cancer (TaT1 and carcinoma in situ)-a summary of the 2024 guidelines update. Eur Urol. 2024;86:531-49.
2. Rink M, Robinson BD, Green DA, et al. Impact of histological variants on clinical outcomes of patients with upper urinary tract urothelial carcinoma. J Urol. 2012;188:398-404.
4. Jain A, Mittal D, Jindal A, et al. Incidentally detected squamous cell carcinoma of renal pelvis in patients with staghorn calculi: case series with review of the literature. ISRN Oncol. 2011;2011:620574.
5. Kumar S, Tomar V, Yadav SS, et al. Primary squamous cell carcinoma of kidney associated with large calculus in non-functioning kidney: a case report. Urol Case Rep. 2016;8:4-6.
6. Perez-Montiel D, Wakely PE, Hes O, Michal M, Suster S. High-grade urothelial carcinoma of the renal pelvis: clinicopathologic study of 108 cases with emphasis on unusual morphologic variants. Mod Pathol. 2006;19:494-503.
7. Hassan M, Qureshi A. Incidental squamous cell carcinoma of the renal pelvis in a non functioning kidney that was missed on two non-contrast CT-scans. J Ayub Med Coll Abbottabad. 2017;29:489-92.
8. Rouprêt M, Babjuk M, Burger M, et al. European association of urology guidelines on upper urinary tract urothelial carcinoma: 2020 update. Eur Urol. 2021;79:62-79.
9. Moher D, Shamseer L, Clarke M, et al. ; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
10. Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res. 2012;22:1435-43.
11. Howick J, Chalmers I, Glasziou P, et al. Explanation of the 2011 Oxford Centre for Evidence-Based Medicine (OCEBM) Levels of Evidence (Table). Available from: https://www.cebm.ox.ac.uk/files/levels-of-evidence/cebm-levels-of-evidence-2-1.pdf. [Last accessed on 5 Dec 2025].
12. Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med. 2018;23:60-3.
13. Sözer IT. Squamous cell carcinoma and calculi in ureteral stump: 12 years post-nephrectomy. J Urol. 1968;99:264-5.
14. Leong CH, Lim TK, Wong KK, Ong GB. Carcinoma of the renal pelvis: an analysis of the diagnostic problems in 23 cases. Br J Surg. 1976;63:102-6.
16. Howat AJ, Scott E, Mackie DB, Pinkerton JR. Adenosquamous carcinoma of the renal pelvis. Am J Clin Pathol. 1983;79:731-3.
18. Mhiri MN, Rebai T, Turki L, Smida ML. Association between squamous cell carcinoma of the renal pelvis and calculi. Br J Urol. 1989;64:201-2.
19. Narumi Y, Sato T, Hori S, et al. Squamous cell carcinoma of the uroepithelium: CT evaluation. Radiology. 1989;173:853-6.
20. Sheaff M, Fociani P, Badenoch D, Baithun S. Verrucous carcinoma of the renal pelvis: case presentation and review of the literature. Virchows Arch. 1996;428:375-9.
21. Kimura T, Kiyota H, Asano K, et al. Squamous cell carcinoma of the renal pelvis with inferior vena caval extension. Int J Urol. 2000;7. 316-9; discussion 320.
22. Kim TS, Seong DH, Ro JY. Small cell carcinoma of the ureter with squamous cell and transitional cell carcinomatous components associated with ureteral stone. J Korean Med Sci. 2001;16:796-800.
23. Sivaramakrishna B, Aron M, Ansari MS, et al. Squamous cell carcinoma of the renal pelvis manifesting after percutaneous nephrolithotomy for long standing calculus. Int Urol Nephrol. 2004;36:149-51.
24. Ham BK, Kim JW, Yoon JH, et al. Squamous cell carcinoma must be considered in patients with long standing upper ureteral stone and pyonephrosis. Urol Res. 2012;40:425-8.
25. Verma N, Yadav G, Dhawan N, Kumar A. Squamous cell carcinoma of kidney co-existing with renal calculi: a rare tumour. BMJ Case Rep. 2011;2011.
26. Paonessa J, Beck H, Cook S. Squamous cell carcinoma of the renal pelvis associated with kidney stones: a case report. Med Oncol. 2011;28 Suppl 1:S392-4.
27. Di Battista L, Stio F, Guarino S, et al. Squamous cell carcinoma of the renal pelvis with stones and inferior vena cava infiltration. Case report. G Chir. 2012;33:182-185.
28. Kalayci OT, Bozdag Z, Sonmezgoz F, Sahin N. Squamous cell carcinoma of the renal pelvis associated with kidney stones: radiologic imaging features with gross and histopathological correlation. J Clin Imaging Sci. 2013;3:14.
29. Jongyotha K, Sriphrapradang C. Squamous cell carcinoma of the renal pelvis as a result of long-standing staghorn calculi. Case Rep Oncol. 2015;8:399-404.
30. Xiao J, Lei J, He L, Yin G. Renal calculus complicated with squamous cell carcinoma of renal pelvis: report of two cases. Can Urol Assoc J. 2015;9:E310-2.
31. Nachiappan M, Litake MM, Paravatraj VG, Sharma N, Narasimhan A. Squamous cell carcinoma of the renal pelvis, a rare site for a commonly known malignancy. J Clin Diagn Res. 2016;10:PD04-6.
32. Jakes A, Jani P, Menon M, et al. Renal Squamous cell carcinoma of a native kidney after renal transplant: a case report. Transplant Proc. 2016;48:259-61.
33. Deng S, Zhang B, Huang Y, Li J, Sang S, Zhang W. Case report of primary renal pelvis squamous cell carcinoma coexisting with long-standing calculi in left kidney on 18F-FDG PET/CT. Medicine (Baltimore). 2017;96:e6341.
34. Kartal I, Uysal S, Adabag A, Gok A, Sagnak AL, Ersoy H. Aggressive squamous cell carcinoma of the renal pelvis. Niger J Clin Pract. 2019;22:588-90.
35. Sun X, Li Y. Incidental squamous cell carcinoma of renal pelvis presenting as skin invasion: a case report. J Med Case Reports. 2020;14:244.
36. Hosseinzadeh M, Mohammadzadeh S. Primary pure squamous cell carcinoma of kidney associated with multiple stag horn stones. Int Med Case Rep J. 2020;13:261-3.
37. Chaurasia Z, Agarwal S, Gupta R, Khatana PS. Pelvicalyceal squamous cell carcinoma: incidental diagnosis with liver metastasis on follow up. Cureus. 2021;13:e18345.
38. Terakawa K, Sawa N, Mizuno H, et al. Renal squamous cell carcinoma-related polymyositis in a patient with autosomal dominant polycystic kidney disease. Intern Med. 2021;60:1237-42.
39. Oh CK, Kim JY. Primary squamous cell carcinoma of the kidney parenchyma with ascending colon invasion: a case report and literature review. Int J Surg Case Rep. 2022;91:106762.
40. Liu XH, Zou QM, Cao JD, Wang ZC. Primary squamous cell carcinoma with sarcomatoid differentiation of the kidney associated with ureteral stone obstruction: A case report. World J Clin Cases. 2022;10:11942-8.
41. Patel AM, Patel J, Jansari T, Thorat R. Incidentally detected primary squamous cell carcinoma of the kidney: case series with review of the literature. J Cancer Res Ther. 2023;19 Suppl:S928-31.
42. Priyatharsan K, Balagobi B, Heerthikan K, Thulasi T, Priyanka A, Sureska G. A rare case of renal squamous cell carcinoma presenting with psoas sign. Int J Surg Case Rep. 2023;110:108732.
43. Alnefaie ZA, Alsolumany AE, Aljahdali FH, Sulaiman OA, Aljehani SF. Reno-duodenal fistula as a complication of staghorn stones and renal pelvis tumor: a case presentation. Cureus. 2024;16:e60739.
44. Qiao J, Tian C, An L, Hong Y, Huang X, Liu J. Application of warning biopsies in percutaneous nephrolithotomy. Transl Androl Urol. 2024;13:1455-62.
45. Holmäng S, Lele SM, Johansson SL. Squamous cell carcinoma of the renal pelvis and ureter: incidence, symptoms, treatment and outcome. J Urol. 2007;178:51-6.
46. Chow WH, Lindblad P, Gridley G, et al. Risk of urinary tract cancers following kidney or ureter stones. J Natl Cancer Inst. 1997;89:1453-7.
47. Tyagi N, Sharma S, Tyagi SP, et al. A histomorphologic and ultrastructural study of the malignant tumours of the renal pelvis. J Postgrad Med. 1993;39:197-201.
48. Chung SD, Liu SP, Lin HC. A population-based study on the association between urinary calculi and kidney cancer. Can Urol Assoc J. 2013;7:E716-21.
49. Federico A, Morgillo F, Tuccillo C, Ciardiello F, Loguercio C. Chronic inflammation and oxidative stress in human carcinogenesis. Int J Cancer. 2007;121:2381-6.
50. Chen YW, Shen SH, Chang YH, Pan CC. Squamous cell carcinoma arising from a renal calyceal diverticulum. Urology. 2016;95:e5-6.
51. Mizusawa H, Komiyama I, Ueno Y, Maejima T, Kato H. Squamous cell carcinoma in the renal pelvis of a horseshoe kidney. Int J Urol. 2004;11:782-4.
52. Gahagan HQ, Reed WK. Squamous cell carcinoma of the renal pelvis; three case reports and review of the literature. J Urol. 1949;62:139-51.
53. Busby JE, Brown GA, Tamboli P, et al. Upper urinary tract tumors with nontransitional histology: a single-center experience. Urology. 2006;67:518-23.
54. An L, Xiong L, Xu Q, Chen L, Ma K, Huang X. Incidental diagnosis of renal pelvic tumor in patients who underwent percutaneous nephrolithotomy: a report of 6 cases and review of the literature. Urology. 2023;171:64-70.
Cite This Article
How to Cite
Download Citation
Export Citation File:
Type of Import
Tips on Downloading Citation
Citation Manager File Format
Type of Import
Direct Import: When the Direct Import option is selected (the default state), a dialogue box will give you the option to Save or Open the downloaded citation data. Choosing Open will either launch your citation manager or give you a choice of applications with which to use the metadata. The Save option saves the file locally for later use.
Indirect Import: When the Indirect Import option is selected, the metadata is displayed and may be copied and pasted as needed.
About This Article
Special Topic
Copyright
Data & Comments
Data
















Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.