Beyond the double incision mastectomy: a narrative literature review and case series exploring alternative techniques in gender-affirming top surgery
Abstract
The double incision mastectomy with free nipple graft (DIFNG) remains the most widely performed technique in gender-affirming chest surgery. However, as patient goals and models of gender-affirming care have evolved, a more individualized, patient-centered approach has emerged. This study reviews historical and current trends in the literature and retrospectively examines 250 consecutive gender-affirming chest surgeries performed by the senior author to assess the breadth of surgical techniques utilized beyond the traditional DIFNG. A total of 70 cases (28%) employed alternative approaches, including double incision without nipple grafts, keyhole, buttonhole, nipple-sparing mastectomy, targeted nipple reinnervation, breast reduction, radical reduction, and mastopexy. These variations reflect a growing diversity in aesthetic, functional, and psychosocial goals, including preservation of nipple sensation, minimized scarring, the option to forgo nipple reconstruction, and maintaining the potential for chest-feeding. This paper outlines the indications and technical considerations for each method and presents a decision-making algorithm to guide individualized surgical planning. As the field of gender-affirming surgery continues to evolve, expanding the operative toolkit is essential to support patients across the gender spectrum and deliver affirming, patient-specific outcomes.
Keywords
INTRODUCTION
Gender-affirming mastectomy is the most frequently performed procedure in gender-affirming surgical care, with the double incision with free nipple graft (DIFNG) technique remaining the most common approach worldwide. However, as models of gender-affirming healthcare have continued to evolve towards more personalized, patient-centered approaches to care, there has been a growing need for a broader range of surgical techniques to better align with diverse transition goals and individual experiences and sources of gender dysphoria. Contemporary gender-affirming chest surgery - or “top surgery” - looks markedly different from what it did even five to ten years ago, as patients increasingly present with more detailed knowledge of a range of surgical options and a wider variety of aesthetic and functional goals. These may include preservation or improvement of nipple sensation, the desire to forego nipple reconstruction altogether, minimization of visible scarring and avoidance of large incisions, breast reduction, or the pursuit of significant chest reduction and contouring without undergoing a full mastectomy.
In this paper, we review the literature as well as the senior author’s most recent 250 gender-affirming top surgery cases to examine the range of techniques employed beyond the DIFNG approach. The aim is to provide an overview of these alternative techniques, discuss their indications, and offer a patient-centered decision-making algorithm to support both providers and patients in selecting the most appropriate surgical approach to meet individualized transition goals. This study highlights the evolving spectrum of gender-affirming chest surgeries, with a focus on techniques beyond the DIFNG, reflecting the increasing personalization of surgical care.
METHODS
A review was conducted of the senior author’s most recent 250 gender-affirming chest surgeries on patients assigned female at birth to evaluate the distribution of surgical techniques used. This study did not involve access to patient records or identifiable personal data; therefore, the principles outlined in the Declaration of Helsinki were followed. All clinical images included in this review are fully de-identified, and informed consent for the use and publication of photographs was obtained from all patients. We also conducted a narrative literature review informed by PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.
Literature review
To assess how contemporary top surgery literature reflects evolving techniques, we performed a PRISMA-informed review of publications from January 2014 to April 2024. We searched PubMed, Scopus, and Embase using terms including “gender-affirming top surgery”, “chest masculinization”, “nipple-sparing mastectomy”, “buttonhole top surgery”, “non-binary chest surgery”, and “targeted nipple reinnervation”. Inclusion criteria were original articles describing surgical techniques or outcomes in gender-affirming mastectomy, in English or French. We excluded case reports with fewer than five patients, editorials, and studies not focused on surgical techniques. The PRISMA flowchart is detailed in Supplementary Figure 1. Articles were screened independently by two reviewers. Reference lists of included studies were also hand-searched for additional citations. As no pooled statistical outcomes are presented, this review is best characterized as a narrative review that integrates available evidence to highlight trends, identify gaps, and provide context for clinical decision-making. This approach allows for a qualitative synthesis of the literature while acknowledging the current limitations of the evidence base and the need for future standardized, multi-institutional research.
Case series
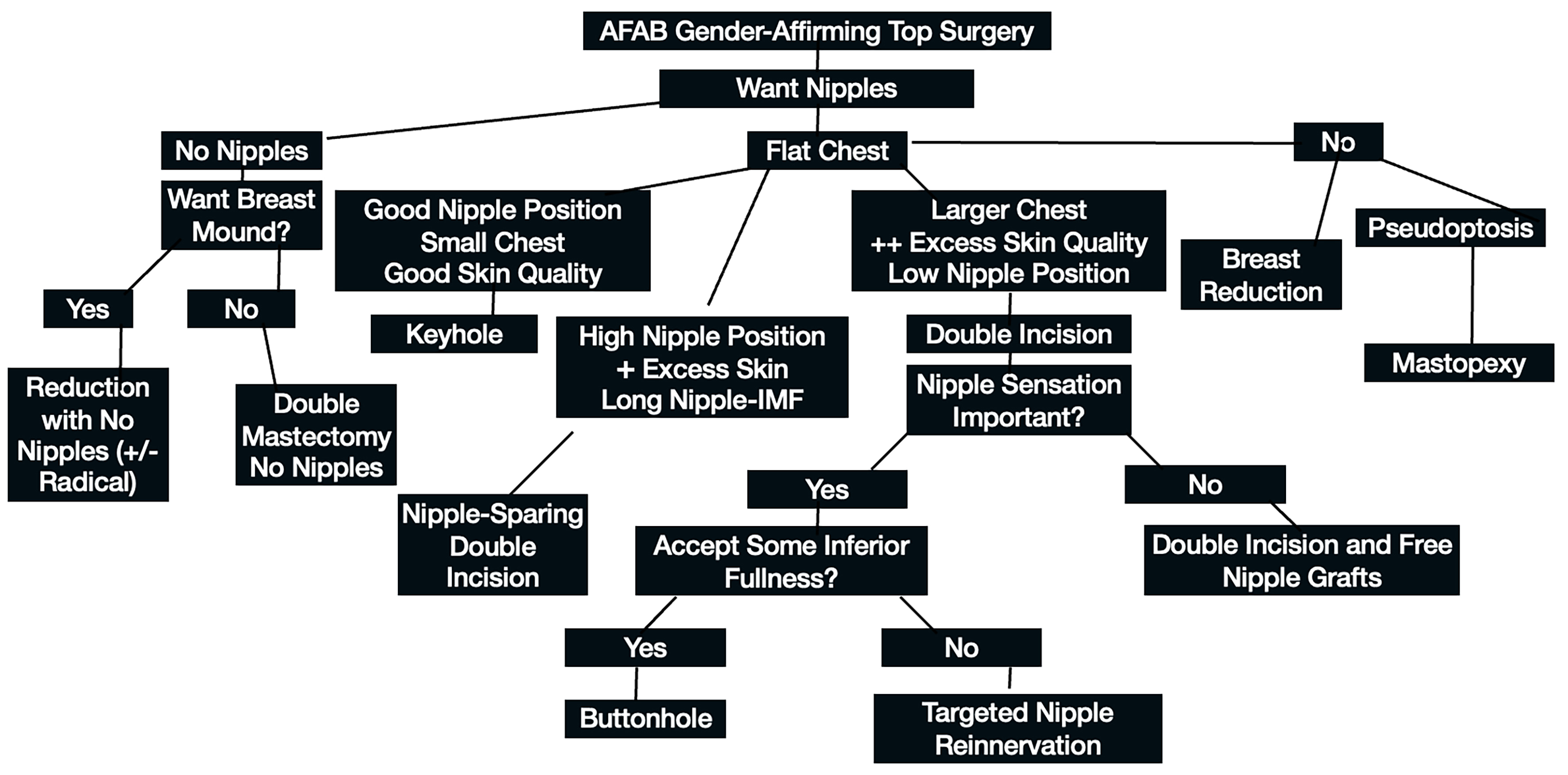
We assessed the proportion of procedures performed using the DIFNG technique compared to alternative approaches, selected based on individual patient anatomy and transition goals. The criteria guiding surgical technique selection are outlined in the decision-making algorithm presented in Figure 1. For patients who underwent an alternative to the DIFNG technique, descriptive statistics were used to quantify the frequency of each surgical variation. A detailed technical overview of these alternative technical approaches to gender-affirming chest surgery is provided.
RESULTS
Literature review
A total of 214 records were identified through database searches of PubMed, Scopus, and Embase. After removing 16 duplicates, 198 records were screened by title and abstract, resulting in the exclusion of 142 studies. The remaining 56 full-text articles were assessed for eligibility, of which 32 were excluded due to wrong population, lack of outcomes, or small sample size (fewer than five patients). Ultimately, 24 studies were included in the qualitative synthesis.
The DIFNG technique has been the most frequently described and widely adopted method, particularly for patients with larger chest size, reduced skin elasticity, or ptosis[1-3]. Numerous studies have demonstrated its consistent aesthetic results and safety profile. Current trends demonstrate a shift away from a standardized DIFNG approach and toward more personalized techniques that reflect patient-specific anatomy, scarring preferences, and gender expression[4,5]. This mirrors broader shifts in gender-affirming care, emphasizing the need to match surgical outcomes with individual goals and identities rather than traditional binary aesthetic norms.
While the DIFNG remains the most studied technique, there has been a gradual rise in the literature focusing on non-DIFNG approaches, including peri-areolar, concentric circular and targeted nipple reinnervation (TNR)[6-9]. However, other techniques have been emerging for patients seeking alternatives to traditionally masculine chest contour. These include buttonhole, radical reduction (central mound, central wedge, wise pattern reduction with nipple grafts), mastopexy and nipple-sparing techniques (inferior wedge)[10,11]. In our experience, these techniques are growing in demand but currently remain published only in case reports or small case series.
Despite these emerging trends, the literature still lacks a robust framework for individualized surgical planning. Few studies systematically address how factors such as gender identity (including nonbinary identification), cultural background, body habitus, or patient-defined outcomes influence surgical decision-making[12].
As top surgery continues to evolve, there is a clear need for future research to prioritize inclusion of non-DIFNG techniques, document decision-making algorithms that support individualized care, and develop validated tools for capturing diverse patient goals. A more comprehensive, patient-centered evidence base is essential for aligning surgical offerings with the full spectrum of gender-diverse identities and expressions.
Case series
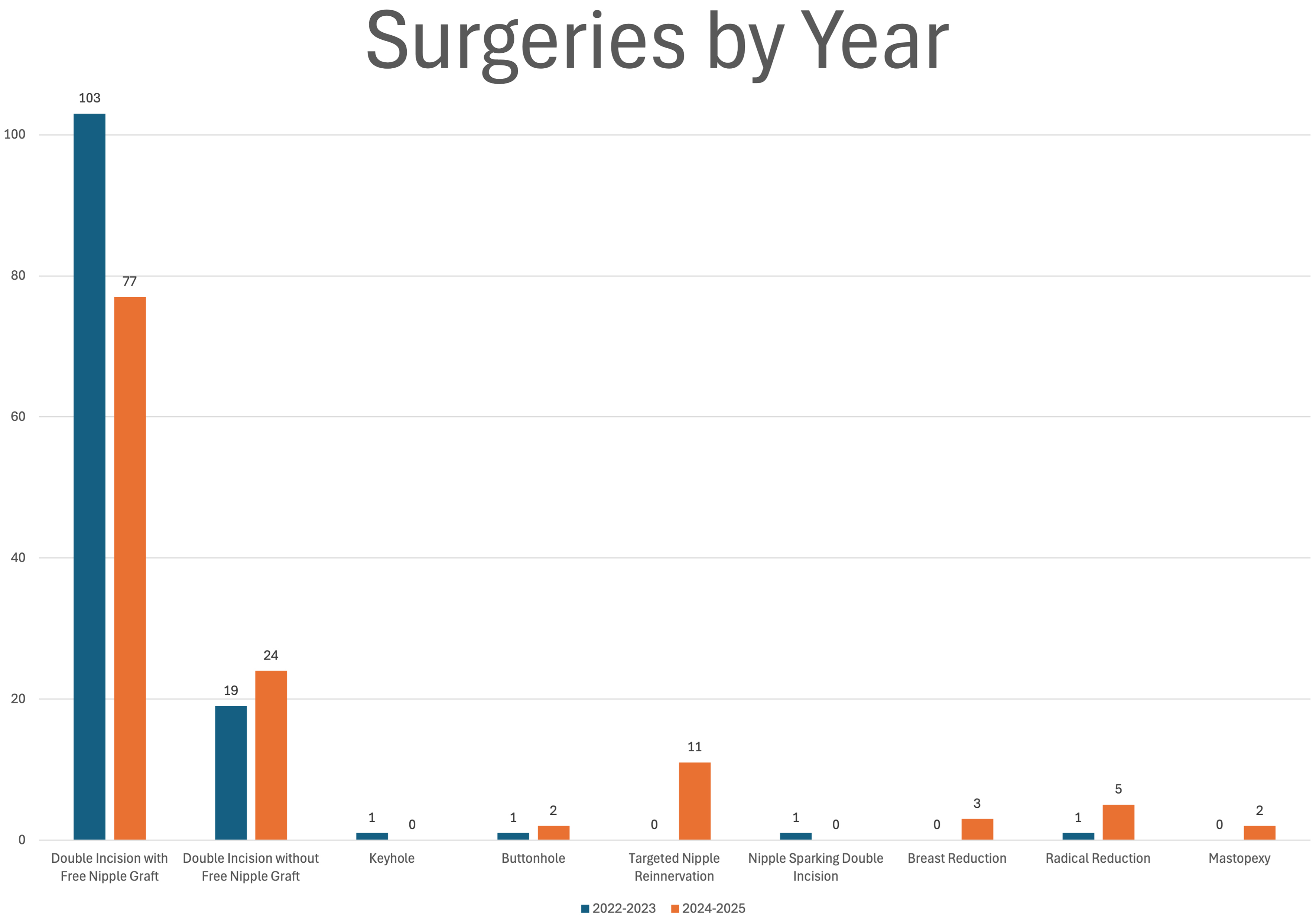
The senior author’s most recent 250 gender-affirming chest cases were performed between August 2022 and April 2025. Of these, 180 were DIFNG and 70 were non-DIFNG (42 double incision without free nipple graft, 1 keyhole, 3 buttonhole, 11 TNR, 1 nipple-sparing mastectomy, 3 breast reductions, 6 radical reductions, and 1 mastopexy) [Table 1]. More recent cases showed a significant trend away from DIFNG with greater variability in technique choice. For example, in the first 125 procedures (2022-2023), 103 were classic DIFNG, whereas in the most recent 125 cases (2023-2025), only 77 were DIFNG [Figure 2].
Figure 2. Distribution of cases demonstrating a trend away from the classic double incision mastectomy with free nipple grafts.
Distribution of cases
| Surgery | Number of cases |
| Double incision with free nipple grafts | 180 |
| Double incision without nipple grafts | 42 |
| Keyhole | 1 |
| Buttonhole | 3 |
| Targeted nipple reinnervation | 11 |
| Nipple sparing double incision | 1 |
| Breast reduction | 3 |
| Radical reduction | 6 |
| Mastopexy | 1 |
| Total | 250 |
Alternative techniques
Double incision mastectomy without nipple grafts
Nipple preservation is a goal for the majority of transmasculine patients seeking affirming chest surgery, but it is not true for all. There is an increasing number of individuals choosing surgical options that deviate from what has been “traditional” or fully binary. As education and awareness of these options have increased, our practice has seen an increasing number of individuals choosing to forgo nipple reconstruction and pursue a nipple-free chest. In a study by Ferrin et al., reasons expressed for this choice ranged from simple and pragmatic choices such as choosing a procedure with a simpler recovery to profound and deeply meaningful choices regarding individual gender expression[13]. Additional factors that influenced patients’ decision to forgo nipple grafts have included an aesthetic that best aligns with gender identity, dysphoria from the presence of nipples and areolae, plans for future chest tattoos, concerns about the aesthetics and outcomes of free nipple grafts, and concerns of nipple loss or increased complications from healing[14-16]. Among these factors, it is important to recognize that some individuals seek out no-nipple top surgery specifically viewing it as a non-binary surgical option. Technically speaking, the mastectomy and skin contouring portion of a double incision mastectomy without nipple grafts is the same as a standard DIFNG without the need to perform nipple reconstruction.
Keyhole surgery
With access to early pubertal suppression, more young adult transmasculine patients may present with limited chest development, often Fischer 1 or 2A[17]. These patients have minimal glandular breast volume and minimal skin excess. If skin elasticity is good and the nipple-areolar complex (NAC) is in an appropriate location overlying the pectoralis major muscle, then keyhole top surgery can provide an unparalleled chest aesthetic[18-20]. The key to this technique is patient selection. In the United States, where 70% of the adult population is overweight or obese, keyhole top surgery can be a relatively infrequent technique. Performing keyhole top surgery in patients with too much glandular tissue or excess skin with poor elasticity will result in skin rippling, contour irregularities and redundant lower pole skin. This is only corrected with revision surgery which often results in an outcome inferior to that of a primary double incision free nipple graft procedure. Although some patients may present with limited chest development and minimal skin excess, counseling on nipple position is also important. Some trans masculine patients will have a low-lying NAC. If keyhole surgery is performed in this setting, the NAC can lie below the pectoralis muscle and appear as if it is lying on the upper abdomen. This is an important part of patient counseling to ensure this is understood in these clinical scenarios. If patients wish to have the NAC moved superiorly, a DIFNG or buttonhole procedure may be preferable.
One of the technical challenges in performing keyhole surgery can be complete excision of breast tissue through a very small incision, limited to a hemi-areola. Often there is more glandular tissue than initially appreciated, particularly in the lateral and inferior aspects of the breast. We prefer to use a combination of both liposuction and an arthroscopic shaver to aid in flap contouring as this allows a more precise excision of the most lateral and inferior portions of the breast tissue where direct visualization is difficult
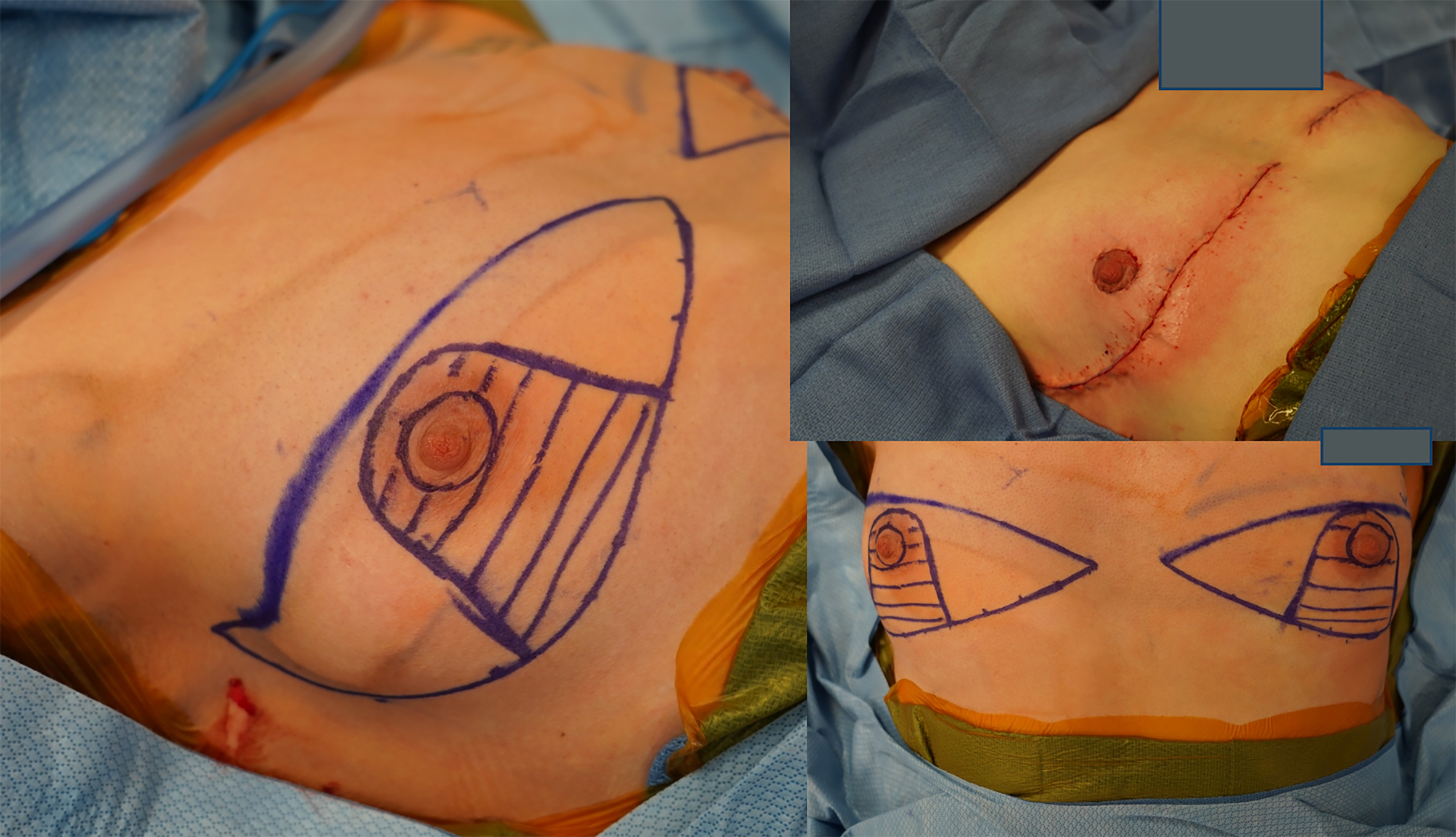
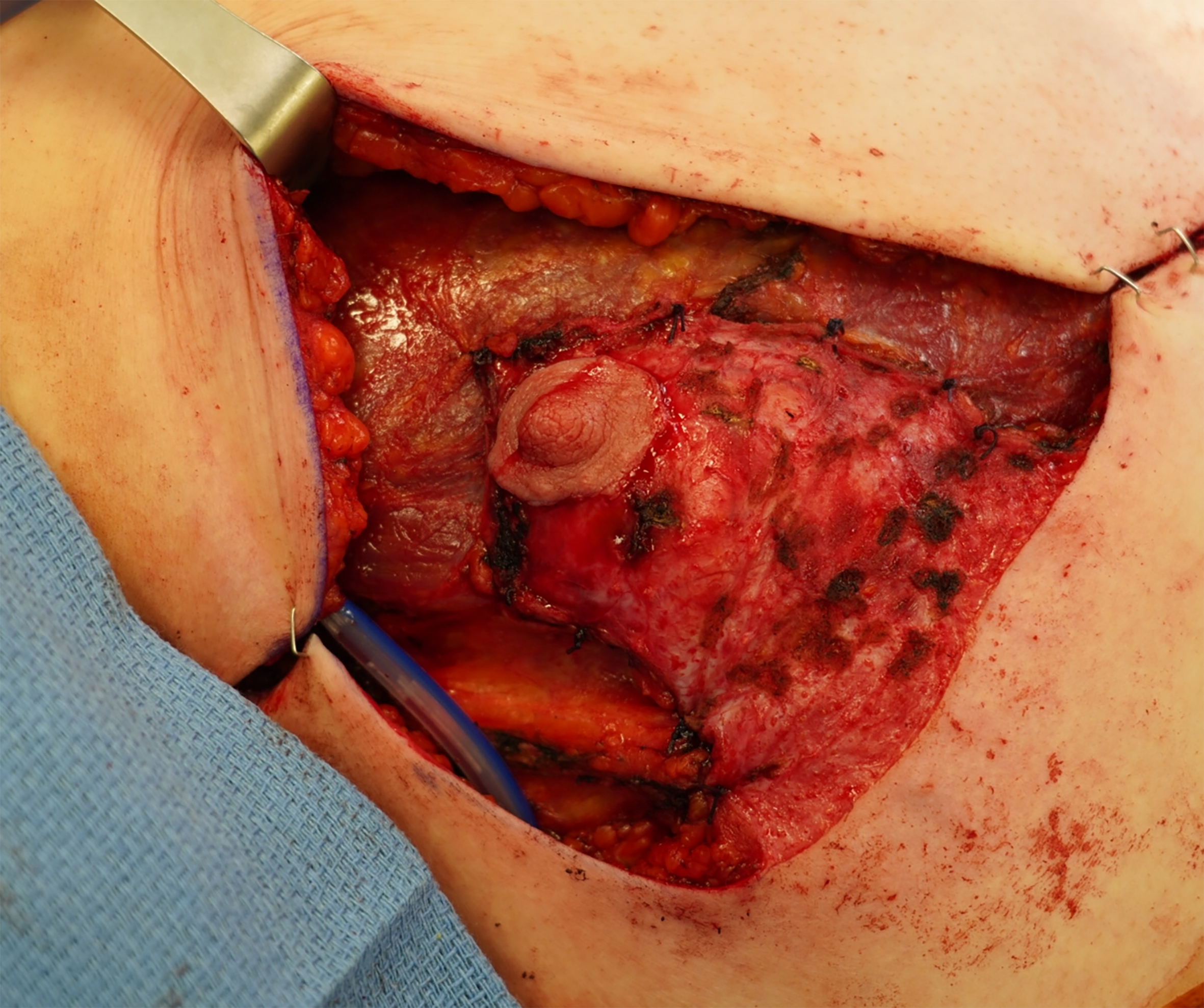
Buttonhole technique
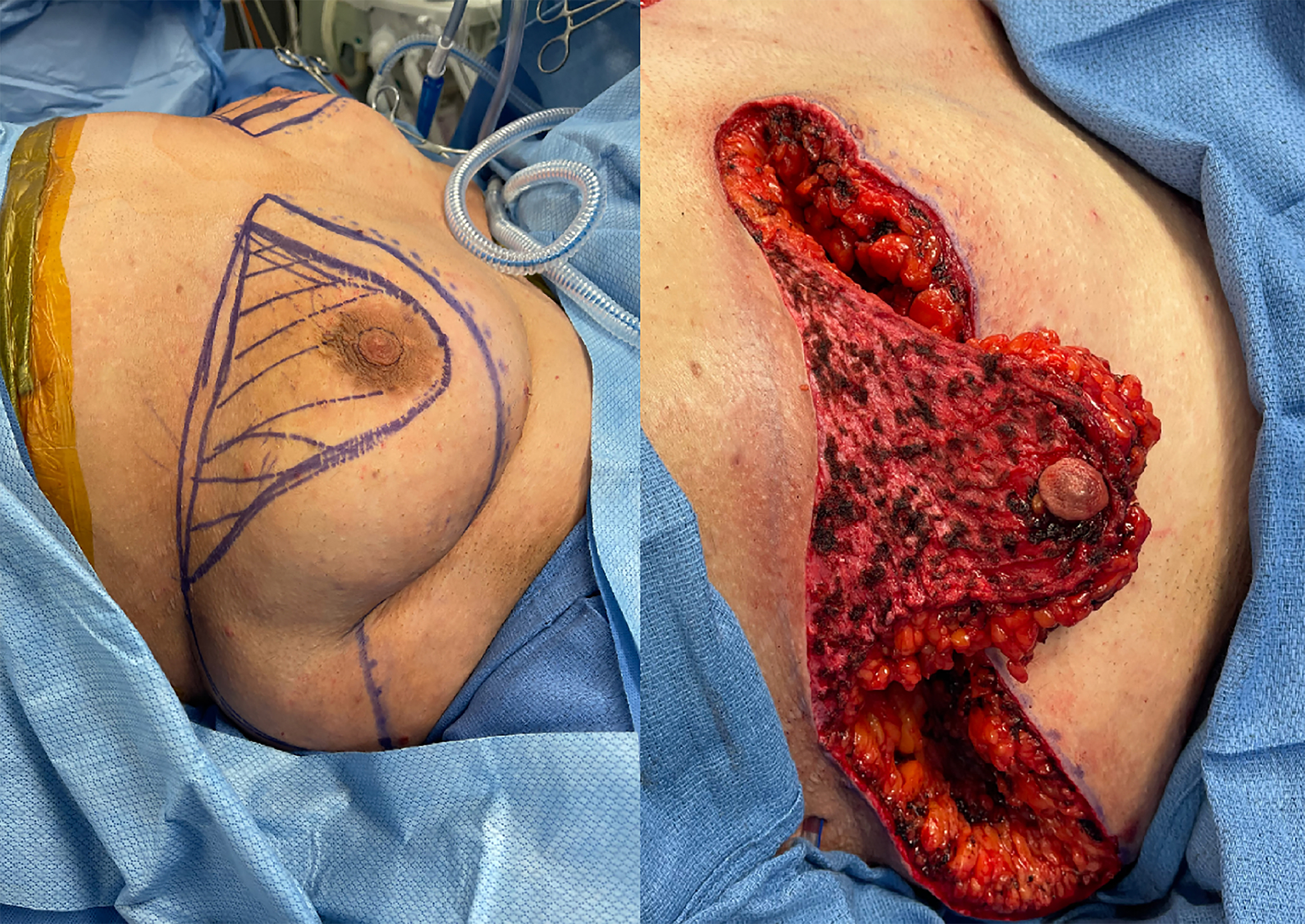
The buttonhole technique consists of a radical breast reduction with resection of all tissue of the lateral, superior and medial breast, while maintaining an inferior-based dermoglandular pedicle to the NAC[18,22,23]. This technique is typically indicated in patients who do not desire a breast mound or more feminine chest shape, but wish to maintain nipple vascularity and sensation to avoid a free nipple graft, and/or do not want a chest that is completely flat. It works best in two patient cohorts: (1) those with broad chests, who are overweight and do not have an excessively long nipple-inframammary fold (IMF) distance and wish to have a chest “proportionally flat” to their body [Figures 3 and 4] and (2) slim athletic patients with minimal glandular tissue volume, moderate skin excess and a short nipple-IMF distance where the pedicle is short and can therefore be thinned extensively to be mostly dermal [Figures 5 and 6].
Figure 3. Buttonhole surgery in a patient with elevated body mass index. The nipple-areola complex is maintained on an inferior pedicle and tissue of the lateral bra roll is maintained in order to create a “body proportion” chest appearance.
Figure 4. Pre- and one-year post-operative photos of a buttonhole surgery - proportional chest appearance following buttonhole surgery in a patient with elevated body mass index.
Figure 5. Buttonhole surgery in a slim patient desiring preservation of nipple sensation and a flat chest contour.
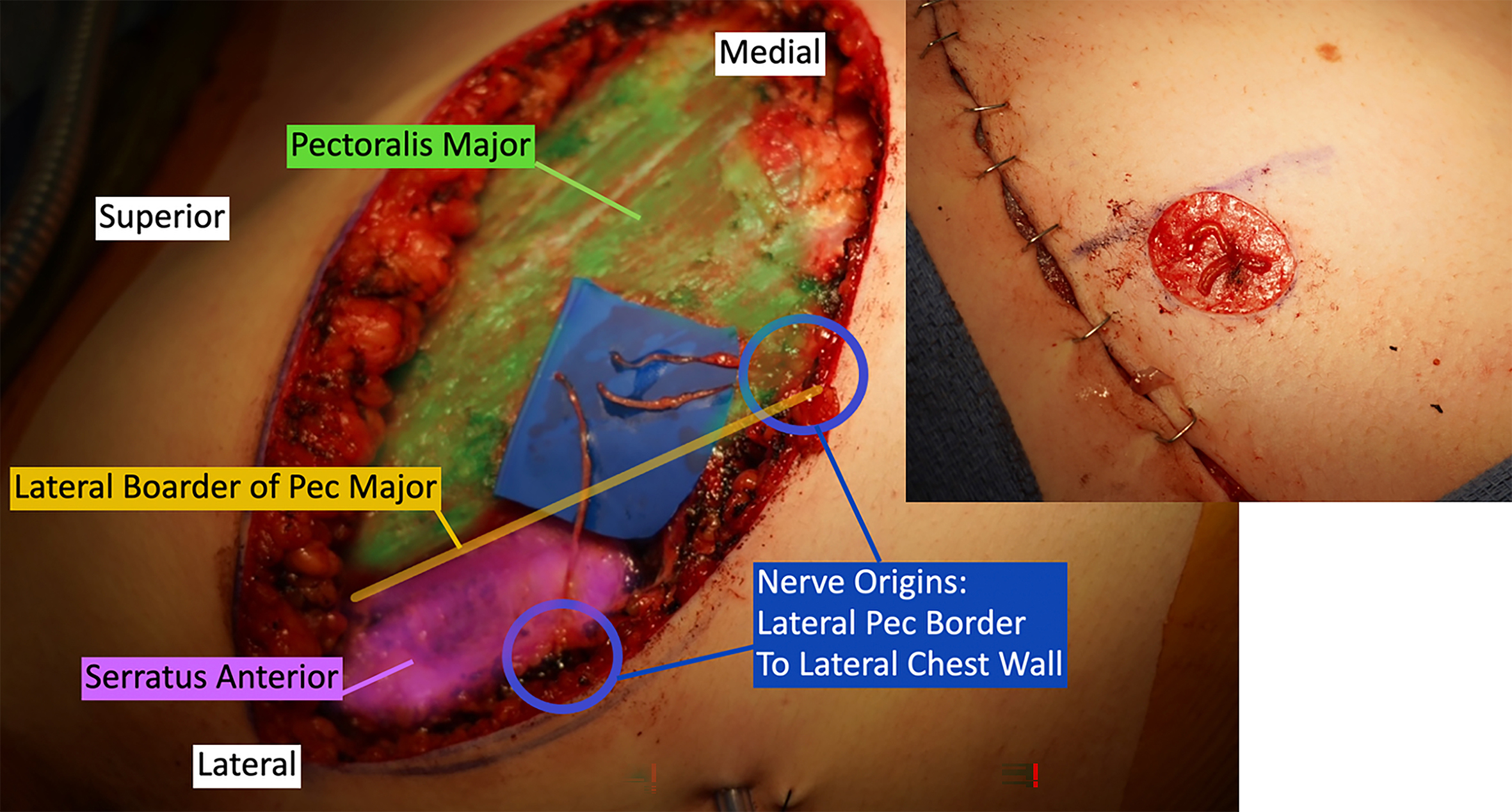
Figure 6. Dermoglandular pedicle in a slim patient undergoing buttonhole surgery. The pedicle is secured to the lateral border of the pectoralis major to hide the fullness of the pedicle and augment the pectoral border.
The buttonhole technique will result in fullness in the lower pole of the chest to maintain perfusion and sensation to the nipple. In slim patients, even a small amount of glandular tissue can compromise a completely flat chest contour, so counseling in this regard is important. It is our preference to secure the dermoglandular pedicle along the lateral border of the pectoralis major with 2-0 Vicryl sutures to flatten the volume of the pedicle as much as possible and orient the volume of the pedicle along the line of the pectoralis [Figure 6]. This camouflages the tissue and at times, augments the appearance of the pectoral muscle. Although it is possible to support the NAC on a dermal pedicle alone to minimize any lower pole fullness, this can increase the risk of NAC loss and significantly reduce nipple sensation. Therefore, in more slender patients who want a fully flat chest contour and to maintain nipple sensation, it is our preference to perform a double incision mastectomy with free nipple grafts and TNR. Patients in larger bodies with a naturally occurring lateral bra roll can have a smooth and cohesive appearance to the chest following buttonhole top surgery, as the tissue of the lower pole pedicle blends smoothly into the lateral chest wall adipose tissue and bra roll [Figure 3]. The final result can be a chest that is “proportionally flat” relative to the patient’s body habitus [Figure 4].
TNR
Achieving desired levels of nipple sensation has emerged as a critical factor for many individuals undergoing top surgery. While certain techniques (i.e., the buttonhole technique) preserve a pedicle to the nipple-areola complex, they may result in post-operative chest fullness due to retained glandular tissue. In order to obtain a flat contour, the majority of gender-affirming mastectomy techniques will involve the use of free nipple grafts. However, this approach often results in the loss of nipple sensation. The innovative technique of nipple neurotization or TNR was first introduced in 2020 by Rochlin et al.[24] and has grown in popularity in recent years with increased patient awareness of this as a surgical option. The procedure involves preserving lateral cutaneous branches of the 3rd-5th intercostal nerves allowing for direct neurotization of the nipple, elongating them with nerve grafts if needed [Figure 7]. Current data support a minimum of two intercostal nerve transfers per side, with direct neurotization being performed when possible or the use of an autologous nerve graft[9]. The most recent sensory data with TNR show promising results. In a prospective study by Remy et al., at one year postoperatively, all patients reported return of NAC and chest sensation, with 88% regaining some degree of erogenous sensation[25]. NAC and chest sensation were significantly improved compared with preoperative values at 12 months, particularly when direct coaptation of two or more intercostal nerve branches was performed. Our team recently published a video paper demonstrating the technical steps of how to perform TNR[26].
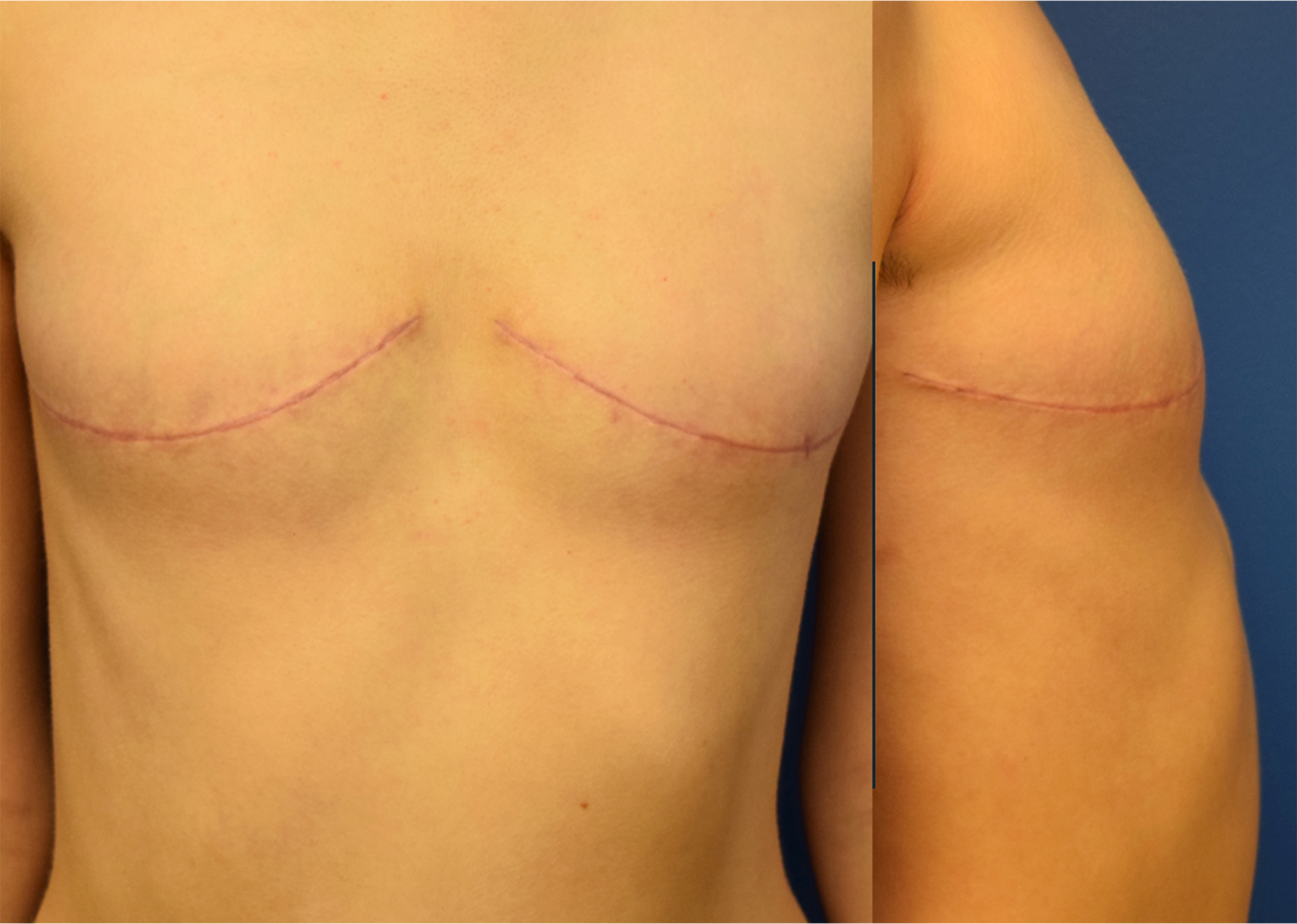
Nipple-sparing double incision
Some patients with a smaller chest, often those classified as a Fischer 2b, will have too much breast tissue and lower pole skin excess to be a suitable candidate for keyhole top surgery[27]. In these patients, a double-incision approach is often necessary in order to adequately remove all of the breast tissue and contour the skin. However, the pre-existing nipple position and areolar size should be closely assessed. Patients with a high nipple position, where the nipple is overlying the pectoralis major muscle, with a long nipple-IMF distance, can often avoid the need for a free nipple graft[28,29]. This not only allows for a simpler surgery and easier recovery but also maintains some nipple sensation and preserves areola pigmentation and nipple projection. In this technique, a nipple-sparing mastectomy is performed, placing the upper incision below the NAC, along the lower border of the pectoralis muscle [Figure 8]. Slightly more skin can be excised in the infero-lateral aspect of the mastectomy if some modest lateralization of the NAC is desired. A nipple reduction can be performed at the same time or as a separate staged procedure under local anesthesia, if desired.
Breast reduction
Modern models of gender-affirming care increasingly recognize gender diversity and the uniquely individual experience of gender dysphoria. Patients suffering from gender dysphoria have a wide range of identities and desired surgical outcomes, and in recent years, there has been a rise in gender-affirming procedures that are not fully binary. One example is gender-affirming breast reduction, which involves performing a standard breast reduction, as for any cisgender patient with macromastia, but specifically to address gender dysphoria. In some patients, the procedure treats both gender dysphoria and the symptoms of macromastia.
Although breast reduction can be an excellent option for many non-binary and transmasculine patients who do not want a flat chest, some patients seek a reduction much greater than what standard pedicled techniques preserving the NAC can achieve. In our experience, it is important to review photos with patients requesting breast reduction and have them bring examples of their desired chest size to ensure that a standard pedicled reduction will meet their goals. For patients seeking a reduction beyond the limits of standard pedicled techniques, the option of a radial reduction approach can be discussed.
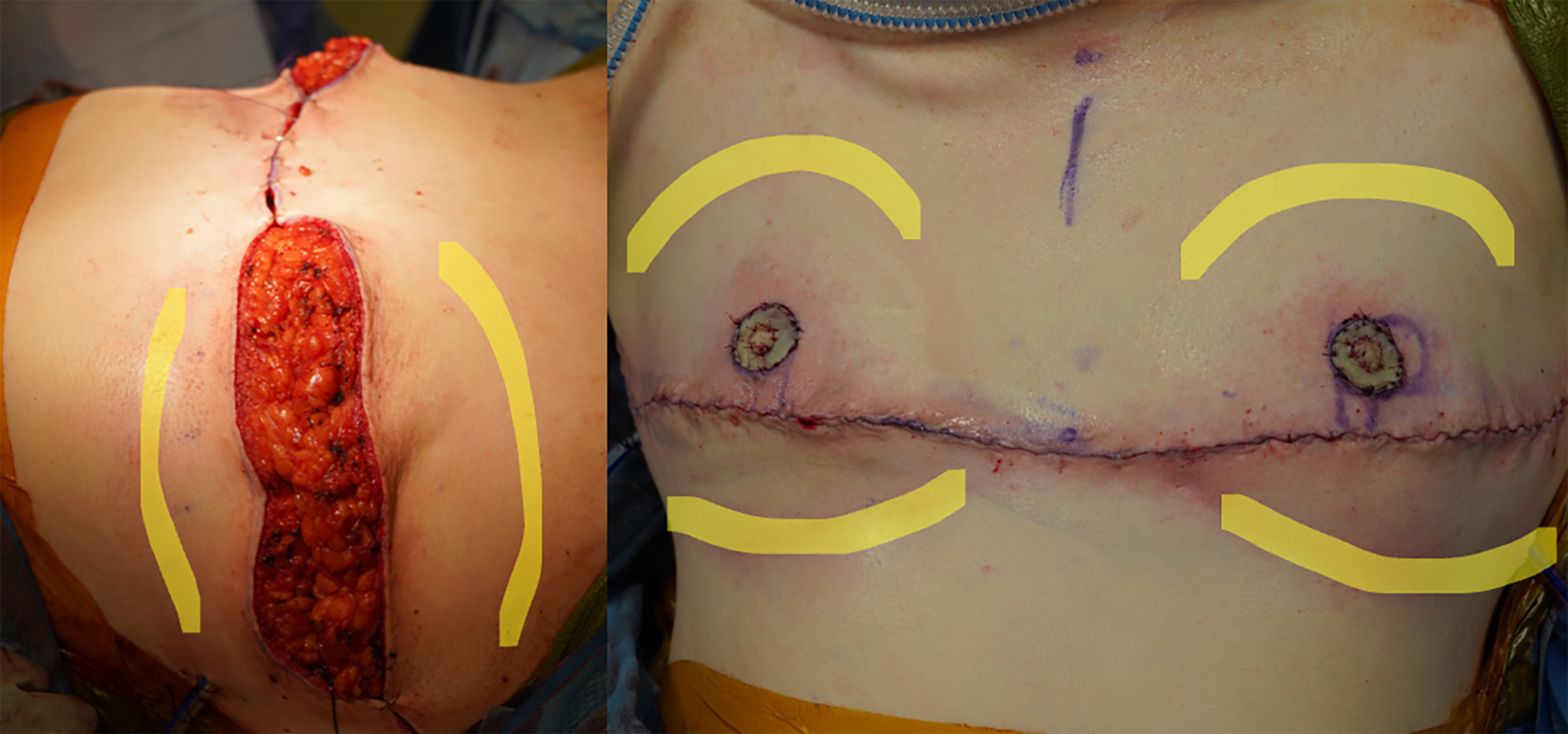
Radical reduction
An increasingly common occurrence in gender-affirming top surgery practices is a patient coming in requesting “not fully flat” or a “radical reduction”. This often represents a gray area between a standard breast reduction technique and full mastectomy top surgery. Understanding precisely what the patient means by these terms is critical, as there is a wide spectrum of possible outcomes between these two approaches. Having patients bring photographs of their desired results, particularly from individuals with a similar body size, is invaluable for accurately assessing their goals.
In our experience, most patients using the terms “not fully flat” or “radical reduction” present with very large chest sizes, often well in excess of a DD cup, and request a “small A cup chest”. Typically, there is a lack of understanding regarding the limits of a pedicled standard breast reduction technique. It is important to show patients photos of breast reduction outcomes, where an A cup chest is generally not achievable from an extremely large chest while maintaining nipple perfusion and sensation. Often, patients bring photos of smaller-bodied individuals with A cup breasts or surgical results that are just shy of fully flat.
In these instances, we discern the desired chest shape of the wanted “A” cup. If the patient wants a breast mound/shape, it is our preference to perform a radical reduction with a central wedge technique, removing all breast tissue except for the upper pole and 2-3 cm of tissue superior to the IMF. This maintains the natural upper pole and lower pole landmarks of the breast, maintaining a natural breast shape [Figure 9]. This technique has not been reported in the literature; however, other techniques for radial reductions have been recently cited[23,28,29]. Patients may then choose to either undergo or forgo nipple grafting [Figure 10].
Figure 9. Radical reduction surgery with nipple preservation. The upper and lower poles of the breast are preserved with a large central wedge excision to create a proportionally balanced “A” cup chest. The nipple and areola are decreased in size significantly to create a more gender-neutral appearance of the chest.
Gender-affirming mastopexy
Although rare, there are a small number of transmasculine non-binary patients who suffer from chest dysphoria but have the desire for future pregnancy and the ability to chest-feed. Although these patients may eventually be interested in a full mastectomy procedure, they may present to discuss “intermediary” options to help treat their gender dysphoria but maintain the ability to chest-feed in the future[30]. Techniques such as a buttonhole procedure do not maintain the sub-areolar glandular tissue and will not maintain any chest-feeding capacity. In these patients, a breast reduction may be one option. In our experience, some patients will present with small to moderate-sized chests, where a significant reduction would potentially result in an inability to chest feed. Understanding exactly where patients’ dysphoria originates can be helpful in designing an individual surgical plan. For patients uncertain about desire for a breast reduction, mastopexy or mastectomy, it is important to counsel patients on the irreversible nature of mastectomy vs. the ability to convert a prior breast reduction or mastopexy procedure to a mastectomy in the future. We have successfully converted many patients with prior breast reductions to a double mastectomy with free nipple grafts.
LIMITATIONS
This study represents a single-surgeon review conducted at a single institution, introducing selection bias and potentially weak external validity. It is important to note that the geographic region in which these procedures were performed may have a distinct demographic profile - likely a higher proportion of non-binary patients compared to binary transgender individuals relative to other regions globally. As such, our results should be interpreted within this context, and further multi-institutional or collaborative studies are needed to validate these findings across diverse populations and practice settings.
This review is primarily descriptive and was not designed to provide comparative outcome data such as complication rates, revision rates, or patient reported outcome measures (PROMs). While inclusion of these measures would strengthen the evidence base, it was beyond the scope of this narrative review. Our goal was to summarize techniques reported in the literature and to highlight less commonly used approaches, drawing on our experience with a high proportion of non-binary patients. Future studies incorporating quantitative outcomes and patient-reported measures such as the GENDER-Q will be essential to further evaluate these techniques. Additionally, our review intentionally encompassed the last ten years to highlight the evolution of individualized and alternative approaches beyond the traditional DIFNG. While this temporal scope may exclude earlier reports, it reflects our focus on capturing the shift in practice patterns and the emergence of novel techniques described in more recent years.
CONCLUSIONS
As patient goals and expectations in gender-affirming chest surgery continue to diversify, surgical approaches must also evolve to meet them. While the DIFNG remains the most commonly performed technique, a growing array of alternative procedures offers more tailored solutions that align with individual aesthetic, functional, and psychosocial priorities. In this study, we reviewed the literature and the senior author’s most recent 250 gender-affirming chest surgeries, detailing the variety of techniques employed and key technical considerations for each. As the field advances, it is imperative that surgeons remain familiar with the full spectrum of operative options to provide truly patient-centered care and achieve optimal, individualized outcomes.
DECLARATIONS
Acknowledgments
Figure 1, Figure 2 and Supplementary Figure 1 were created in Microsoft PowerPoint.
Authors’ contributions
Contributed to study design, research, and manuscript composition: Bonapace-Potvin M, Isbester KA, Chen RH, Peters BR
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
All clinical images included in this review are fully de-identified, and informed consent for the use and publication of photographs was obtained from all patients.
Copyright
© The Author(s) 2025.
Supplementary Materials
REFERENCES
1. Monstrey S, Selvaggi G, Ceulemans P, et al. Chest-wall contouring surgery in female-to-male transsexuals: a new algorithm. Plast Reconstr Surg. 2008;121:849-59.
2. Ammari T, Sluiter EC, Gast K, Kuzon WM Jr
3. Wolter A, Diedrichson J, Scholz T, Arens-Landwehr A, Liebau J. Sexual reassignment surgery in female-to-male transsexuals: an algorithm for subcutaneous mastectomy. J Plast Reconstr Aesthet Surg. 2015;68:184-91.
4. Raner GA, Shapiro JS, Tse T, Armstrong K, Potter E. Binary and nonbinary transgender patient experiences accessing gender-affirming top surgery. Plast Reconstr Surg Glob Open. 2024;12:e6198.
5. Hu AC, Liu MT, Chan CH, et al. Gender affirming surgery in nonbinary patients: a single institutional experience. Arch Plast Surg. 2023;50:63-9.
6. Wilson SC, Morrison SD, Anzai L, et al. Masculinizing top surgery: a systematic review of techniques and outcomes. Ann Plast Surg. 2018;80:679-83.
7. Kuruoglu D, Alsayed AS, Melson VA, Figueroa NS, Fahradyan V, Martinez-Jorge J. Masculinizing chest wall gender-affirming surgery: clinical outcomes of 73 subcutaneous mastectomies using the double-incision and semicircular incision techniques. J Plast Reconstr Aesthet Surg. 2023;85:515-22.
8. Rifkin WJ, Robinson IS, Kloer C, et al. Gender-affirming mastectomy: comparison of periareolar and double incision patterns. Plast Reconstr Surg Glob Open. 2022;10:e4356.
9. Truong AY, Chinta M, Chen Y, Black GG, Valerio IL, Gfrerer L. Targeted nipple reinnervation in gender-affirming mastectomy using autologous nerve graft. Plast Reconstr Surg Glob Open. 2023;11:e5203.
10. McTernan M, Yokoo K, Tong W. A comparison of gender-affirming chest surgery in nonbinary versus transmasculine patients. Ann Plast Surg. 2020;84:S323-8.
11. Schafer RE, Fodor R, Marlar R, et al. Nonbinary and transgender male patient preferences for gender-affirming top surgery. Ann Plast Surg. 2024;93:e36-44.
12. Bertrand AA, DeLong MR, McCleary SP, et al; Plastic Surgery Research Group. Gender-affirming mastectomy: psychosocial and surgical outcomes in transgender adults. J Am Coll Surg. 2024;238:890-9.
13. Ferrin PC, Pua E, Isbester K, Peters BR. Factors affecting the choice to forgo nipple grafts in gender-affirming chest surgery. Ann Plast Surg. 2024;93:189-93.
14. Rahmani B, Park JB, Adebagbo OD, et al. Along the spectrum from reduction to mastectomy: comparing the opinions of an online transmasculine and gender-diverse community on an algorithmic approach to gender-affirming top surgery. Aesthetic Plast Surg. 2025;49:4332-42.
15. Garvey SR, Friedman R, Nanda AD, et al. Along the continuum from reduction to mastectomy: an algorithmic approach to the gender diverse top surgery patient. J Plast Reconstr Aesthet Surg. 2023;83:246-9.
16. Cuccolo NG, Kang CO, Boskey ER, et al. Masculinizing chest reconstruction in transgender and nonbinary individuals: an analysis of epidemiology, surgical technique, and postoperative outcomes. Aesthetic Plast Surg. 2019;43:1575-85.
17. Bluebond-Langner R, Berli JU, Sabino J, Chopra K, Singh D, Fischer B. Top Surgery in Transgender Men: How Far Can You Push the Envelope? Plast Reconstr Surg. 2017;139:873e-82.
18. Tang A, Hojilla JC, Jackson JE, et al. Gender-affirming mastectomy trends and surgical outcomes in adolescents. Ann Plast Surg. 2022;88:S325-31.
19. McEvenue G, Xu FZ, Cai R, McLean H. Female-to-male gender affirming top surgery: a single surgeon’s 15-year retrospective review and treatment algorithm. Aesthet Surg J. 2017;38:49-57.
20. Top H, Balta S. Transsexual mastectomy: selection of appropriate technique according to breast characteristics. Balkan Med J. 2017;34:147-55.
21. Bramati ML, Palacios Huatuco RM, Garcia Rodriguez B, Dolino F, Mayer HF. Ultrasound-assisted liposuction for top surgery in transgender men: clinical experience and evaluation of satisfaction and quality of life with TRANS-Q and BREAST-Q. Aesthetic Plast Surg. 2025;49:1290-8.
22. Beaufils T, Berkane Y, Freton L, et al. A new surgical technique for female-to-male top surgery: the posterioinferior pedicle (PIPe) approach. Aesthetic Plast Surg. 2023;47:2283-94.
23. Swanson E. Comparative outcome study of gynecomastia surgery and gender-affirming mastectomy with 100% nipple preservation. Ann Plast Surg. 2025;95:e1-17.
24. Rochlin DH, Brazio P, Wapnir I, Nguyen D. Immediate targeted nipple-areolar complex reinnervation: improving outcomes in gender-affirming mastectomy. Plast Reconstr Surg Glob Open. 2020;8:e2719.
25. Remy K, Alston C, Gonzales E, et al. Targeted reinnervation during gender-affirming mastectomy and restoration of sensation. JAMA Netw Open. 2024;7:e2446782.
26. Peters BR, Bonapace-Potvin M, Dhami JK, Hathaway BA, Shepard E. Targeted nipple reinnervation in gender-affirming mastectomy: a “how to do it” technical primer. Plast Reconstr Surg Glob Open. 2025;13:e6657.
27. Krakauer KN, Balumuka D, Meza-Rochin A, Rapp K, White E, Hansen J. Addressing the gray zone in affirmative mastectomy: an analysis of fischer 2 patients. Ann Plast Surg. 2023;91:376-80.
28. Robinson IS, Salibian A, Zhao LC, Bluebond-Langner R. Nipple-preserving inferior-ellipse mastectomy: a new technique for gender-affirming top surgery. Plast Reconstr Surg. 2024;154:237e-40.
29. Tse T, Potter E, Armstrong K. Techniques for preserving the nipple areolar complex in chest masculinization for all chest sizes. Cureus. 2025;17:e80757.
Cite This Article
How to Cite
Download Citation
Export Citation File:
Type of Import
Tips on Downloading Citation
Citation Manager File Format
Type of Import
Direct Import: When the Direct Import option is selected (the default state), a dialogue box will give you the option to Save or Open the downloaded citation data. Choosing Open will either launch your citation manager or give you a choice of applications with which to use the metadata. The Save option saves the file locally for later use.
Indirect Import: When the Indirect Import option is selected, the metadata is displayed and may be copied and pasted as needed.
About This Article
Special Topic
Copyright
Data & Comments
Data



















Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.